Yael’s 20 years with CLL have been “as good as it could be”
Yael Morris was very young – only 34 years old, 28 weeks pregnant, and living in Darwin – when she was diagnosed with CLL 20 years ago.
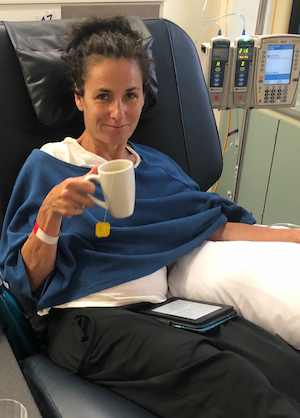
After being on watch and wait for many years before having standard therapy (FCR*), today Yael is doing well on ibrutinib (Imbruvica®) which is controlling her CLL.

The stunning spot where she lives at the base of Mt Macedon with her husband, Greg, her poodle, Louis, and many noisy chickens, provides her with the peace she particularly appreciated and needed while going through treatment.
Diagnosed in Darwin but choosing to be treated in Melbourne
Though filled with ups and downs, Yael describes her 20-year journey with CLL as, “as good as it could be”.
It began with a blood test, a routine full blood examination as part of her pre-natal care, and Yael and Greg were spending a few days out of town when she received a phone call asking her to come in for follow-up blood tests when they returned to Darwin.
“They suspected I had CLL because my lymphocyte count was suspiciously elevated during the pregnancy,” said Yael, recounting the lead-up to her diagnosis in July 2001. Further tests showed that the cells were all of the same line.
At the time, Yael was employed by Territory Health, coordinating the breast screen program there, and Greg was an aeromedical doctor based at Darwin Hospital.
“We were in shock. There was no haemato-oncologist in Darwin at the time and the physician I saw didn’t give me a great outlook,” said Yael.
“We rang friends in Melbourne, where I’m originally from, and was recommended a haematologist.”
The couple travelled to Melbourne to meet with Professor Schwarer (Tony) and to have further ultrasounds, “to make sure my baby was okay”.
Yael’s disease was not staged until December 2001, after she gave birth.
“At that time, it appeared that the CLL wasn’t aggressive and my doctor was very positive. I liked him and I’ve been seeing him ever since,” said Yael.
“And that’s my message. The importance of finding a doctor you can connect with, who you can be open and honest with, and someone who works for you.”
“He never promised me anything; with the nature of the disease, it’s very difficult, and he couldn’t say what would happen in the future, but he always promoted living for today.”

Yael and her family left Darwin in late November 2001, moving to regional Victoria, and finally settling in the Macedon Ranges an hour away from Melbourne and their extended family.
Did Yael have undiagnosed CLL the previous year?
Yael had a benign breast lump a year before her CLL diagnosis.
“Even though I’d been diagnosed at 34, I wondered if I’d had CLL longer,” she said.
“I mentioned this to my haematologist, and they were able to redo the pathology on the frozen section which determined a mono-clonal B-cell infiltrate. That led to the conclusion that I’d probably had CLL for at least a year before the actual diagnosis.”
Yael was told her CLL prognosis was, “pretty good, but we still didn’t know what that would mean”.
Getting on with life on watch and wait
Yael was on watch and wait and her daughter, Noa, was born at the end of September 2001.
“I’ve only had one child because of my diagnosis,” said Yael, now aged 54.
“There was very little research about young people with CLL. I think there was probably one case written up in the medical journals.”
Yael’s appointments with her haematologist were monthly before stretching out to every three months, then eventually to twice a year, before becoming more regular as the disease progressed.

“Every time I had an appointment, we’d look at my health markers, blood count, lumps and bumps, and we’d discuss the disease,” said Yael.
“We’d also discuss the latest research, we’d discuss conferences my doctor had attended, we’d discuss things they were trialling. I wasn’t ready for treatment, but he’d always discuss that with us.
“Of course, I was nervous before each appointment.
“I learnt how to do self-hypnosis to prepare for childbirth and have kept the practice to manage the anxiety I get because of my diagnosis. I believe that any cancer, especially a blood cancer, is systemic and affects all of me.
“I looked at what I would need to maintain my health, not that eating organic food and exercising would cure the CLL, but it would help my head-space and how I managed myself.
“I also felt self-hypnosis would be good and brought it up with my GP. Part of what she incorporated into my self-hypnosis was trusting my treatment team.
“I had my mantras, which I used when I was giving birth, whenever I had a bone marrow biopsy or a CT scan, and I still practice self-hypnosis,” said Yael.
She is a qualified teacher, whose career path had taken her from teaching to community work for local governments and health promotion. In the Macedon Ranges, Yael worked for the local council, did community work, managed her husband’s medical practice, some retail work, and a stint in a restaurant.
“I tried travelling into Fitzroy for work when my daughter was young but decided against it as the travel was onerous, so I tried my hand at lots of different things,” said Yael.
“I was always interested in dissemination of health information and the importance of health literacy.”

Yael got all her information about CLL initially from speaking to her haematologist.
“For years, I didn’t want to Google a lot as I feared not being able to differentiate another’s experience from my particular disease status,” Yael explained.
“My doctor has given me journal articles to read at times and to discuss when approaching that pointy end towards disease management.
“I’m not into some brochures hospitals may give out and I can’t remember if my doctor even gave me a brochure about CLL. I think dialogue is really important, also having an extra person with you during your medical appointment and taking lots of notes. I usually go to each appointment with a list of questions.
“In the early days, when we had lots of questions and we didn’t understand a lot, we would email my haematologist, and he’d email us back the same day.
“I could have Googled from time-to-time but stopped because sometimes you see worst case scenarios.”
During the 14 years Yael was on watch and wait, she lived a healthy life and focused on being well.
“That meant having a full life working, being involved in community activities, eating well – we’ve got a great veggie garden – going for walks, doing yoga, and being physically fit,” said Yael.
“I tried to lead as normal a life as I could.”
“At times I would worry, and in the early days I did have my fears. I may not have shared them with anyone, but I’ve had my quiet moments where I’ve laid on the couch or in bed and cried. I think that’s normal when you reflect upon things,” said Yael.
“But once you become a mum, you become busy with your child and juggling work, volunteer commitments, and child-rearing.
“And I had a lot of faith in my doctor and in sharing information and being part of the decision-making process… asking questions when I meet with him.

“When I needed to speak to him, if I was ever worried about anything, I’d make an appointment to see him.
“I didn’t want to be a passive patient.
“For years, Tony would say, ‘patients with CLL, it can creep up on them and they don’t realise’. In a way he was trying to make me aware and to pick up cues, so I was able to report back.”
When Yael’s CLL started to progress
About six years ago, when Yael started getting tired, perhaps from having the disease for so long, she began having Intragam® (immunoglobulin) infusions.
“We’ve played around with the frequency over the years – four-, five- or six-weekly – depending on how I was feeling and checking my IgG** levels. At the moment, I have it every four weeks.”
Yael’s CLL level in her bloods remained good, although “it would go up and down a bit”.
“Even when I needed treatment, they weren’t at that crazy level that other CLL patients’ lymphocyte counts are at,” she explained.
“There are times when you worry. You worry if your glands are up for a while and something doesn’t feel right… things like that, and I was a glandy CLL patient.”
Yael’s disease became more active around three years ago.
“My glands were huge. I had lost a lot of weight and ended up with a massive spleen and liver.
“It was then that Tony said he felt that I’d need treatment soon and that it was better for me to choose the time, rather than later when I’m forced to have it.”
In January 2019, Yael began the standard of care treatment, FCR, which she had over six months.
“It reduced the CLL count in my blood quite quickly, and by the end of the treatment, no CLL was detected in my blood but once I had my bone marrow biopsy, there were still some remains in my bone marrow.”
Her haematologist suggested ibrutinib as her next line of treatment.
“He would have liked me to start earlier, but I chose to have a break and not be on anything for a couple of months.
“Noa was doing VCE that year and I’d gone to Melbourne for treatment, so the year was already pretty disruptive for her.”
How speaking to the Leukaemia Foundation helped
“I was scared about starting another treatment modality, so I contacted the Leukaemia Foundation and spoke to Katherine Treble, a blood cancer support coordinator, who was fabulous and helped me.
“We had a great chat and it de-mystified the process. She speaks to lots of patients who have been on FCR or who are on ibrutinib. It was a wonderful counselling session.”
Yael had developed a sore on her temple during FCR which she kept forgetting to mention to her haematologist, but eventually she did.
“Katherine rang one morning as I was going to see a plastic surgeon skin specialist. I told her, ‘I think I may have a BCC [basal cell carcinoma]’, and she called me back that afternoon to double-check on me.
“Even though Tony was saying to me for years, ‘you’ve got to be careful in the sun’ and explained that incidence of another primary cancer was higher when you have a cancer, I didn’t take the information in. It was from speaking to Katherine that I realised the direct link between CLL and BCC.
“I think people say the same things to you and you hear different people at different times.”
At the end of 2019, Yael begin taking ibrutinib, three tablets a day and it’s controlling the CLL.
“I still have CLL. I don’t have lumps and bumps at present, but I do have side effects; the tummy cramps that lots of people have, muscle weakness, and I have put on weight.
“I still see Tony every couple of months and if I need to see him more regularly, I do.
“I’ll stay on ibrutinib until it doesn’t work anymore, and then we move to another therapy,” said Yael.
“I’m a long termer, that’s how I look at it.”
The hugeness of CLL
“Being diagnosed was huge and treatment was huge, but you know FCR is for a finite period, so you live for that period to be over,” said Yael.
“I kept moving. I walked and did pilates daily, made sure I ate and I practised self-hypnosis which kept me calm. I visualised the drugs destroying the cancer.
“I read literature and I use that to calm me. I find losing myself in literature reduces my anxiety.
“Friends and family made us beautiful meals. My daughter performs, so listening to her sing was really beneficial. You focus on getting through it, then living through it.
“I can see by the blood test results that the disease is under control at the moment with ibrutinib. It hasn’t gone away but it’s controlled, and that’s huge. Modern medicine is incredible,” she said.
How COVID-19 has affected Yael
“COVID has had a huge impact on me, it’s brought out another set of fears,” said Yael.
“I was always careful prior to treatment. My husband would tease me because when I travelled, I’d wear a mask and I’d wipe things down because I didn’t want to pick anything up as I was already immune compromised.

“Last year was stressful. We had to bring our daughter back from overseas, and my husband shifted out for several months as he works in a hospital and didn’t want to expose me to whatever he might come into contact with.
“I couldn’t go in to see Tony, my doctor, last year. If I felt I had a bug I was too scared to go in as I didn’t want to pass it on to him or patients in the waiting room, so we had lots of telephone appointments.
“I have always exercised and was incredibly fit prior to starting treatment, but today I only want to exercise with people who are immunised and that isn’t guaranteed,” said Yael.
When Yael spoke to CLL News, she’d recently had her first shot of the Astra Zeneca COVID-19 vaccine and her daughter had come home from Melbourne, where she is studying arts, to stay with her parents during the most recent lockdown.
While Noa has always known her mum to have CLL, Yael said, “as the disease became more active and as she became an older teen, I think it has affected her. She has fears to do with her mum’s mortality, but I think that’s what happens when a parent is ill”.
Right now, Yael says, “I’m someone who has had a chronic condition for 20 years”.

“Sometimes, when you get to my age and you have CLL, it’s like, ‘is it CLL or is it menopause?’, you know?”
But she’s not worried about the future, “as there is too much to look forward to in the here and now”.
“I’ve decided to worry only when things go wrong. I love living one day at a time where today everything’s fine.”
* FCR is a combination of the chemotherapy drugs, fludarabine and cyclophosphamide, and the targeted therapy, rituximab.
** Immunoglobulin G (IgG) is a blood antibody that is part of the immune system and helps to fight off infections.
Last updated on July 21st, 2021
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.