The ups and downs of leukaemia… ‘one day at a time’

Geoff Hamilton was diagnosed with acute monocytic myeloid leukaemia (AMML), a sub-type of AML, almost four years ago. In this first-person narrative, Geoff shares his experiences. His shock diagnosis, relocating to another state for treatment, going through a stem cell transplant, recovery, returning home, going back to work, and the present – dealing with graft versus host disease – a significant after-effect of his life-saving therapy.
“When I was diagnosed with leukaemia midway through 2017, I was completely blind-sided.
“For a fit and healthy 55-year-old, who had never been in hospital overnight since birth, this was a shock. Having digested the news, my first response to my local GP (at Campbell Town, Tasmania – a town of just 770 people) was, “what do I need to do?”.
“Having passed on the terrifying news to my wife, Jan, I then rang a good friend (and paediatrician) at Wagga Wagga (NSW), our home for the previous 25 years, and asked him what I should do.
“He requested a copy of my blood results, confirming the white blood cells had moved off the ‘Richter scale’ at 93, and summed up my situation. ‘You will need two or three rounds of chemotherapy and a bone marrow transplant to survive this’, he said.
“Of course, I had no idea what this meant. He then proceeded to make enquiries about getting me re-located to Royal Melbourne Hospital (RMH) to receive the best treatment possible. He had worked with many children with leukaemia over the years and was up-to-date on how and where to be treated.
“The first few days were a complete blur… lots of tests, discussions, and meetings with specialists (and of course, their trainee registrars).
“I was diagnosed with acute monocytic myeloid leukaemia (AMML) with a FLT 3 mutation.
“Jan made a decision early on to be by my side for the entire process. After my initial diagnosis, she quickly returned to our home to pack a few bags and neither of us returned for over 12 months. Luckily, we had friends and helpers who kept an eye on things.
“Unbeknown to me, Jan became my ‘advocate’ from Day 1 – questioning doctors, writing things down, researching information on my condition, and keeping family and friends updated on the news.
“Early-on in the process I made the decision to write a blog primarily to keep family and friends informed of my treatment. This process was, strangely enough, very helpful in my recovery. It gave me a daily goal – to put 500 words and a few photos together. Something that would normally be an easy task but in the early stages of my illness was a mammoth exercise!
“My paediatrician friend, John, advised me to assign tasks to family members, saying, ‘they will want to help, so give everyone a job!’.

“On this advice, I allocated ‘food and fashion’ to our daughter, Claire. She was to kit me out in ‘hospital clothes’, not of the PJ type, but more sports/leisure wear including bright socks and undies! Being a foodie, she was more than happy to cook up wonderful meals and bring them into my ward at 7B in RMH. Hospital food is not always the most inviting!
“Our son, Lachlan, was tasked with ‘IT’ for my stay in hospital, setting up the blog, getting photos taken, setting up music and movies and a reliable internet connection.
“And our youngest, Dougall, was given the job of ‘livening up my room’ – basically putting up a myriad of photos of family and special memories, and well wishes from friends that had come in via email and text. He covered every wall in my room!
“In the early stages I asked my first consulting haematologist, Professor John Seymour, if he had managed to see a few people in recent times with my strain of leukaemia survive. His positive answer was certainly enough to give me hope. I was going to be his next one!
“My journey was generally straightforward for the first six months prior to my stem cell transplant (SCT) or bone marrow transplant (BMT). Luckily, my brother, Tony, was a perfect match which saved the need for a worldwide search for a donor. Unfortunately. I contracted a nasty lung infection after my second round of chemotherapy which took many IV doses of Ambisome to rectify. How little did I know that this might have been what ended my life!
“My experience post-BMT was one of ups and downs. The first 100 days are critical, although the medical team simply says it is a key target to look out for. What they mean is, ‘if you survive this period, there is a good chance you will live’. I had 17 blood transfusions in the 10 months post-transplant, plus severe diarrhoea and other complications. At one stage I was taking 44 tablets a day.

“Depending on what you read and who you talk to, the survival rates for my type of leukaemia are around 50-60%, based on recent research. This was the figure my post-BMT haematologist, Dr Amit Khot provided, based on a recent research paper. I was happy to work with these odds, believing that being better than 50% I had a good chance of recovery. If I had of googled the same question, the 27% survival rate quoted on the internet may have left me a little despondent!
“Now that I am three years post-BMT and have received a ‘full clearance’ from my haematologist, I consider myself to be one of the fortunate ones. There is no doubt that modern medicine can achieve remarkable results. Once upon a time, if you were older than 45, you were not offered a bone marrow transplant.
“I generally feel well most days, but still suffer from tiredness and fatigue. I got down to just two tablets daily – absolute bliss!
“The main issue I deal with is GVHD (graft versus host disease) which has moved from bowel issues, to lungs, liver, kidneys, and now mouth and muscles. For quite some time, my GVHD issues were at the ‘margin’ – all of which are minor in the scheme of things. My haematologist advised that they could not predict the future impact of GVHD which affects everyone differently.
“The main issue now is sclerodermatous skin, which has gradually degraded over a period of six months, mostly during the COVID pandemic. Many appointments were by telehealth rather than in person (not ideal for a skin condition).
“My blood testing frequency has increased, as has the cocktail of drugs used to fight this condition. I was back up to as many as 30 tablets a day (with all the associated side effects), which has been a big backwards step, but a necessary one to fight the current disease. Sometimes it is difficult to accept this ‘down’ when things have been going so well. In addition, I was treated with ECP (Extra Corporeal Photopheresis) which has been very effective, reducing the fibrosis of my skin which was becoming quite worrying.

“I can do most, if not all, of the tasks and activities that I enjoyed prior to my diagnosis. I am back at work and love the challenge of processing information and planning ahead. There was a time during my treatment when I couldn’t read a newspaper, let alone a book. Jigsaws were about as much as I could manage.
“As a private pilot, one of my biggest goals was to return to flying. I was advised this would take some time and it was with a great sense of achievement that I returned to flying approximately two years after my first treatment.
“Of course, during a two-year period of treatment, you have lots of time to contemplate life. From the outset, when I engaged with the thought of death, I came to the position that I had no regrets. There was no huge list of things I felt I’d missed out on or not yet done. I felt I was close to family and friends.
“In fact, I put my recovery down to three simple things:
- Excellent medical advice and treatment. The staff and consultants at Royal Melbourne Hospital and Peter McCallum were absolutely wonderful and very dedicated. The medical professionals always appeared to have time for you, no matter how busy they were.
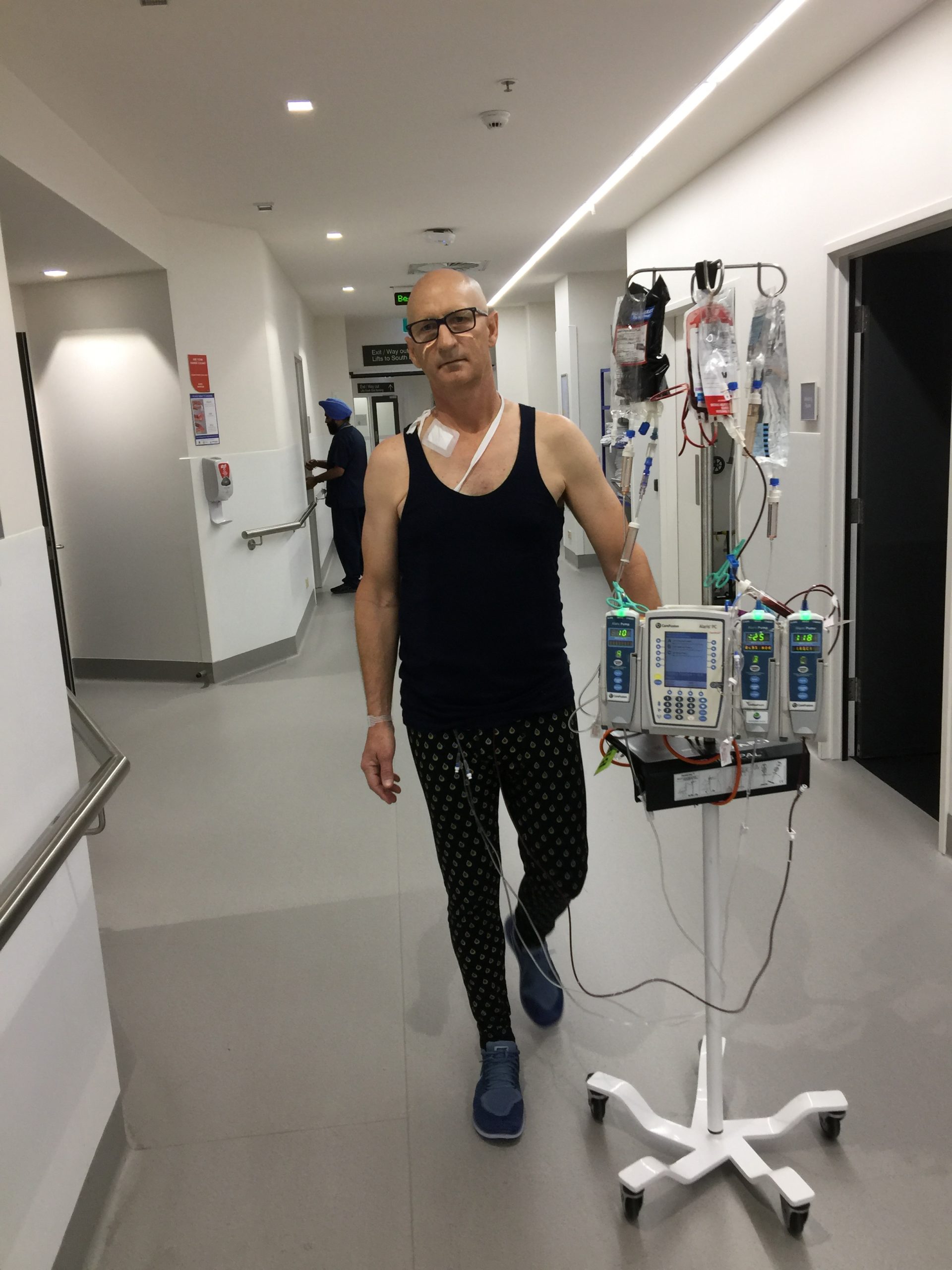
- My goal setting for small, and then larger tasks, included regular exercise, whether it be just getting out of bed four times a day to walk the ward or getting back into the gym. My mantra for many months was simply, ‘one day at a time’.
- The support and contact from family and friends, through messages on my blog and regular visits in hospital. Never underestimate how important this can be for recovery.

“My wife and I have always sought information to clarify situations and my medical treatment was no different. We researched as much information as possible and I often provided summaries of such on my blog, to help people understand what was happening. I have probably now completed a partial degree in haematology. Not bad for someone who previously did not know what a platelet or neutrophil was! I am sure my doctors got somewhat tired of my questions.
“I have attended many Leukaemia Foundation meetings in Melbourne and Launceston, now that we are home again. I have found these to be very helpful in meeting other people who have experienced similar treatment and outcomes. In fact, through friends I have been able to make contact with several other AML patients throughout Australia and have cherished the opportunity to share stories and learn from others’ experiences. I think it is the unknown that scares us most, and if we can picture what we might go through it helps with our mental disposition.
“For now, I am looking forward to returning to (an almost) normal life. I enjoy business, flying, sport, farming and spending time with family and friends. Going through a process like this allows you to focus on the important things in life and re-set your priorities.”
You can read about my thoughts in my blog: geoffbeatsleukemia.com

Last updated on June 23rd, 2021
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.