Mogamulizumab being considered again by PBAC
This month the Pharmaceutical Benefits Advisory Committee (PBAC) will consider a resubmission from Kyowa Kirin for mogamulizumab (Poteligeo®) for relapsed or refractory (R/R) cutaneous T-cell lymphoma.
The Leukaemia Foundation made comments to the July 2020 PBAC meeting for a previous submission for mogamulizumab (when the PBAC made a first-time decision not to recommend) and again for the November 2020 PBAC meeting.
The requested listing is a Section 100 (Efficient Funding of Chemotherapy) Authority Required (Written) listing for patients with R/R CTCL who have been previously treated with at least one prior systemic therapy.
The Leukaemia Foundation’s Head of Policy and Advocacy, Emily Forrest, said, “we understand that patients with early-stage MF are treated primarily with skin-directed therapies, whereas patients with treatment-resistant early-stage MF, advanced-stage MF, or SS require systemic drugs including vorinostat, or cytotoxic chemotherapeutic drugs”.
“We understand that in the MAVORIC clinical trial, mogamulizumab significantly prolonged progression-free survival compared with vorinostat. Also, patient-reported outcomes, as measured by the Skindex-29 and FACT-G, showed significantly greater symptom reduction and improved functional status in favour of mogamulizumab versus vorinostat in early cycles and throughout treatment.
“We also requested consumer feedback via the Leukaemia Foundation’s disease-specific Facebook pages, which included a link to the Patient Voice Initiative ‘Tip sheet for submitting consumer comments to the PBAC’,” said Ms Forrest.
The Leukaemia Foundation received one response to its request for feedback for the July meeting from consumers: Donna, a CTCL patient in Queensland who we understand has not undertaken treatment with mogamulizumab: I’ve not been given any drugs and I’m asking WHY when I’m at Stage 4 … .
“A second request, for the November meeting, did not receive any consumer comments, which may reflect the small population of patients for this therapy to date,” said Ms Forrest.
Information provided by the Leukaemia Foundation to the PBAC in support of the two submissions included: “CTCL is a rare type of lymphoma, and rarer still for specific subtypes of the disease such as MF and in particular SS. Smaller patient populations with rare diseases face significant hurdles in accessing new treatments in a timely manner. It is for precisely this reason that patients and clinicians need access to new therapies to treat the disease.
“We therefore urge the PBAC to consider the high unmet needs of this patient population in its decision making and in making a recommendation to government for listing this therapy on the PBS.”
More PBAC news on CTCL
In other PBAC news, on 1 November 2020, methoxsalen (Uvadex®) was listed on the Pharmaceutical Benefits Scheme (PBS) for patients with erythrodermic CTCL who have not responded to other treatments.
Methoxsalen was approved for listing by the PBAC at its May 2020 intracycle meeting. It was considered as part of a streamlined co-dependent dual-review process with the Medical Services Advisory Committee’s consideration of Medicare funding of extracorporeal photopheresis (ECP) for CTCL, based on a favourable clinical and cost-effectiveness comparison.
Approximately 75 patients annually are expected to benefit from this listing. ECP also will be funded through Medicare for use in combination with methoxsalen.
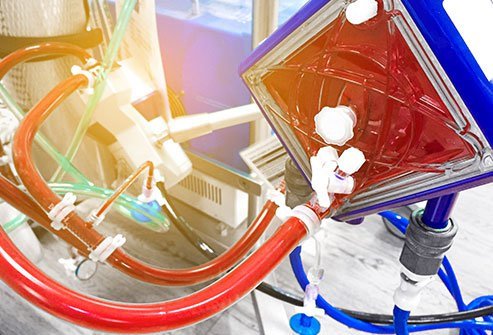
ECP involves attaching a patient to a machine that removes some of their blood, separates the white blood cells (WBC) and returns the red blood cells and platelets to the body. The WBC are mixed with methoxsalen, exposed to ultraviolet light, then administered to the patient, to activate their immune system to fight the blood cancer.