Martin’s setting new records for remission and enjoying life while living with myeloma
During the 22 years Martin Boling has had myeloma, blood cancer of various types has affected four other members of his family too, not just him.
In October 1999, when he first went to Canberra Private Hospital with back pain which turned out to be a symptom of myeloma, Martin was surprised to discover his sister’s father-in-law was in the same ward. He had myeloma and was having a bone marrow transplant.

Four months later, Martin’s younger brother, Adam was diagnosed with acute lymphoblastic leukaemia (ALL) and the following year, by happenstance, “the two Boling brothers were both in the high dependency unit at the same time,” said Martin’s wife, Patricia.
“When I went in to see them, I had to see Martin first before I went to see Adam, who was in a more sterile area,” she explained.
That was in February 2001. Martin was recovering after an autologous stem cell transplant as was Adam, who’d had an allogeneic stem cell transplant. Sadly, Adam died while Martin was still in hospital.
“Martin was barely well enough to be let out of hospital to go to his funeral,” said Patricia.
Another family member, Martin’s cousin, Brett, also was diagnosed with myeloma “about 10 years ago”. And, more recently, Patricia found out she has chronic lymphocytic leukaemia (CLL).
“I thought blood cancer was quite a rare disease, but it’s touched our lives in quite a few different areas,” she said.
Martin’s diagnosis and initial treatment
Martin enjoyed “enviable good health and fitness” until mid-1999 when blood tests to investigate the cause of a swollen lymph duct in his armpit revealed some anomalies and he was diagnosed with MGUS – monoclonal gammopathy of unknown significance. His haematologist told him not to worry.
Three months later, when Martin and Patricia were on a family holiday in Hong Kong, Martin suffered extreme back pain after a jolt on a backroad’s bus trip. When this didn’t improve after returning home to Canberra, Martin saw his GP and a physiotherapist.
“Things went downhill very rapidly,” said Martin.
The pain got so bad it made him sick and when he couldn’t get out of bed, Patricia called the ambulance. He was admitted to hospital, saw a spinal specialist, and had a blood test. He had compression fractures of the lumbar spine and associated renal failure.
But when Martin’s haematologist received his latest blood results, he was sent to the Canberra Hospital immediately and Patricia recalls being told, ‘he’s so ill, he might not make it to Christmas’.
“It had turned from smouldering MGUS in to galloping myeloma within two months,” said Martin, who was 49 at the time and working at the National Health and Medical Research Council (NHMRC).
“I was almost comatose when I was taken by ambulance to hospital for admission. I woke up with a central line – cannula implanted through the chest wall just below the collar bone – and tubes running every which way.”

Martin started treatment immediately, nine courses of VAD* and a short course of radiotherapy.
“During this time, I returned to work on a part-time basis,” he said.
“As a Commonwealth public servant, the provisions for sick leave were very generous and I’d built up quite a bank of it. This meant I could work three weeks out of four.”
He took off the week after chemo, “to avoid opportunistic infections” and in August 2000 Martin had a stem cell harvest – enough for two stem cell transplants.
“I had an autologous transplant in February 2001, leaving enough for a second transplant in the freezer, if required later,” said Martin.
“I made close to a record recovery with discharge from hospital after 13 days.”
Returning to work and normality
Martin returned to work full-time in April 2001, to a more research-based role working on policy that could be done in his own time.
“I certainly wanted to go back to work, and to get back to as close to ‘pre-getting sick’ normal as I could.”
His ongoing medication was a monthly infusion of a bone-strengthening bisphosphonate, and a self-administered injection of interferon three times a week to boost his immune system. He had to live with certain lifestyle limitations, such as giving up gardening, forsaking the gym, and skydiving was out, not that he’d ever done it!
“I had to be careful going downstairs, so I didn’t jar my spine, I looked after my general hygiene, and stayed away from people who weren’t well,” said Martin.
And Patricia said some things were put in place in their household.
“We did everything we could think of to make the house as safe as possible. Tea towels and hand towels were washed every day, bath towels every second day, and we had a diet of fresh food.”
In mid-2001, Martin got pneumocystosis, which Patricia described as “a sneaky kind of pneumonia where you’ve got no phlegm and no cough”.
“Martin was losing weight and we couldn’t find the reason until he had a lung scan, and it took a few months for him to recover,” she said.
Changes in Martin’s health and medication

Martin’s experiences with myeloma were “thankfully uneventful” until December 2005, when he had shingles. This coincided with the emergence of more pain that was initially diagnosed as a disc bulge but turned out to be a myeloma mass.
He was treated with more radiation and his medication was changed. The interferon was stopped and he started taking thalidomide, which rekindled his VAD-induced peripheral neuropathy, along with dexamethasone.
“Peripheral neuropathy is one of those givens that comes from taking thalidomide,” he explained.
“It’s like having pins and needles or numbness in the feet and fingers, and sometimes and I had a bad vague perpetual metal taste on my tongue.”
The peripheral neuropathy steadily progressed and by November 2019 Martin could feel it in his thighs and groin, up to his elbow and sometimes “on the top of my skull”.
His treatment was changed again, from thalidomide to lenalidomide (Revlimid®), on a dose of one tablet every day.
“I very quickly found that it was having some serious side effects, so we stopped it altogether for a while then went on the normal protocol – a tablet every other day for three weeks followed by a week off [in four-weekly cycles],” said Martin.
“I reckon the peripheral neuropathy is a lot less now, so maybe there’s been some regeneration of the nerves.”
At the end of 2021, when Martin’s immune system was very low and he was at risk of catching everything going around, including COVID-19, he started having immunoglobulin monthly.
Both Martin and Patricia have avoided getting COVID.
“We are being very careful. I still get the groceries delivered and if we have to go to a shop, we are very strategic. We go the minute it opens when there are no people there,” said Patricia.
“And we’re wearing masks all the time when we’re out,” added Martin.
How Martin is faring
Martin remembers distinctly, when he was first diagnosed “last century” with quite severe disease, something his oncologist said when he first went to hospital for day treatment.
“As we walked down the ward, he said, ‘oh, this is so and so, she’s had myeloma for 20 years’. She was probably about 70, so in effect he was saying, look, it’s not a quick and deadly disease,” recalled Martin.
“He also said back then that in his experience myeloma was not going to be something that I would just sort of cruise through.
“To some extent, that’s the way I feel I’ve handled it, I’ve just cruised on through. There may have been the occasional flag from the roadside speed camera or the roadside cop saying, ‘oh, hey, hey,” but I’ve gone, ‘no, I’m just keeping on going’ and it’s done me well so far.
“It is my intention to set new records for ‘remission’ and enjoy as normal a life as I can, while I can,” wrote Martin on his Facebook page, back in January 2009, when he reckoned “nine years is a good start”.
“I’ve reconciled that after 22 years I’m doing a hell of lot better than most people,” he says now.
“I try not to let it get me down, but I know I’m living on borrowed time. Even for a member of the normal population to be, as I am, 71 plus years is doing pretty well.
“The last thing my oncologist said recently was, ‘looking at these bloods, you’d never know that you had myeloma’. He’s very pleased and thinks I’m his ‘longest surviving patient’, as in longest living with myeloma, for which I thanked him very gratefully.”
The impact of Martin’s disease on his family
Martin and Patricia’s two sons, Nicholas and Alexander were aged 16 and 14 when Martin was diagnosed in 1999.
“It had quite an effect on them, to have their father so ill and feeling that he might die, and on me, trying to manage at home,” explained Patricia.
“Martin was quite adamant that everything had to continue. The boys had to go to school, to Scouts, to martial arts, and I had to go to work,” said Patricia, a policy adviser in the Federal government.
“As far as possible, life continued as normal for the family, which was quite tricky, fitting in visits to the hospital morning, noon, and night.
“The kindest and most practical thing my work did was give me a car space right near my office, so I could come and go if there was a specialist appointment, or I suddenly got a call from hospital to say the rounds were going to be on early this afternoon,” she said.
“The boys were very affected. Alex was very gentle and calm. He’d never hit anyone in his life except probably his brother, until I got a call from the school to say he’d flattened another child in the playground – a bully who’d monstered some younger kids.”

Patricia’s immediate thought was, ‘who is this child? He’s not mine’.
“And Nick turned out to be the man of the house, helping with the shopping and fixing things including the laundry door. For many months we’d been carrying the washing around the house to the clothesline,” said Patricia.
“It was very interesting to see how teenagers react. They wouldn’t see the school counsellor or any counsellor I suggested, but the wonderful people at the carers’ association recommended someone who was a chiropractor and a counsellor. I sent the boys to him on the pretext of niggling martial arts injuries. He was a very good listener and a very good counsellor for them.”
Throwing a house renovation into the mix
Martin said, “life became interesting” in early 2000 well before his transplant.
“It’s a while before I get back to work, but we decided we needed to do a major renovation of the house. It took 10 months and was finished just before Christmas.”
“I did think, why are we doing this?” said Patricia.
“You know, if he’s going to die and the kids are going to grow up and leave, I’d be rattling around in this extended house. It just added to the excitement really.”
An architect helped, basing the reno around what they needed to change then, and what they thought they’d need in five years and in 10 years.
“It’s worked really well. We still have four bedrooms but put two new bedrooms on for the boys, in the second level, and redid the bathroom so it was friendly for someone who would be disabled,” said Martin, who was in a wheelchair when he first came home from hospital.
“And it’s been great ever since. It’s light and it’s warm because we’ve got double glazing throughout.”
“And it’s easy to clean,” added Patricia.
Retirement and a second blood cancer diagnosis in the Boling household
Martin retired in 2006 just shy of his 55th birthday, thanks to the government’s “very generous superannuation scheme for people who joined the Commonwealth Public Service after leaving school”, as Martin had.
“You get a lump sum payout plus a regular superannuation pension. We used the lump sum to pay off the mortgage which seemed the logical thing to do given my health status, and it’s worked out well,” said Martin.
Patricia continued working until she was 65, retiring two years ago, around the same time she was diagnosed with CLL after a routine annual blood test.
“I was not real happy. I kept it quiet from everyone until I knew what was going on. It’s at stage one and progressing slowly, which is good,” she said.

A year earlier Patricia had been diagnosed with breast cancer which has been treated with surgery, radiation and hormone blockers, no chemo.
“I’m on Zometa® [a bone-strengthener] like Martin. I did have visions that we’d sit together, having our infusions and holding hands in the ward, but we go to different hospitals, so it’s not romantic at all,” said Patricia, who describes her health as “very good at the moment”.
“We’ve been very lucky that our kids have changed jobs and moved back to Canberra. That has meant that through the last two years, when I needed a lot of care and Martin needed some care, they were available and able to help us, and their wives as well, which has been extraordinary.”
Looking back over the last 22 years, Martin says, “it’s been a bit of a rollercoaster” but with more ups than downs, and now he’s enjoying a plateau.
When Martin spoke to Myeloma News, the latest update from his haematologist was “all good”, with no signs of the disease progressing.
What normal life entails now for Martin
These days Martin goes down to a local men’s shed to play cards and three mornings a week he “makes sawdust” which currently involves using some tools in new ways to make a garden bench. As a member of The Growing Friends, he propagates plants from the collection at the National Botanic Gardens, and at home, from his own seed sources, and his front garden is now a mass of native plants.
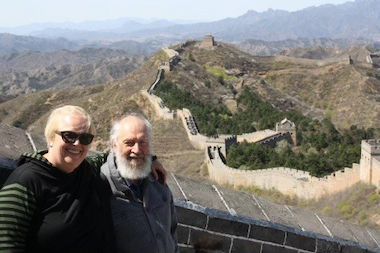
Travel has been a popular pastime for the Bolings, mostly over the last 10 years.
“We’d paid off the mortgage, the kids had left home, and we had a bit of money to spend on ourselves. There’s that golden time,” said Patricia.
The couple has tripped to mainland China, up the Mississippi, to Japan twice, the Baltic states, to Rome, Florence and Paris, and around New Zealand where they plan to go again in early 2023.
Treatment – past, current, and future
Commenting on the Australian Capital Territory and federal health systems, Patricia said, “Martin occasionally gets a glimpse of what some of the medication he takes would cost if you had to pay for it and not get it through the Pharmaceutical Benefits Scheme (PBS), and it’s extraordinary”.

“When he first came home from hospital after his stem cell transplant, he was taking 18 different kinds of medication and there was no way we could have afforded that kind of treatment.
“We’ve been very lucky, and we are grateful for the great specialists, great hospitals, and great GPs who keep it all together and coordinated,” she said.
Looking to the future, Martin said, “it’ll be interesting to see if I get prescribed any of the monoclonal antibodies such as alemtuzumab”.
“There are some exciting things going on in research involving genetic profiling, and CAR T-cell therapy looks very promising.”
“I’m not trained in medical research or in medicine in any way, but because of my background with the NHMRC, I’ve picked up a lot and have become knowledgeable, more so than most people [with myeloma] are.
“Right from day one, because of where I was working, I was able to talk to professors of medicine who were looking at various aspects of treating the disease, including Professor Doherty [Australian immunologist and Nobel laureate] who was instrumental in helping to develop stem cell harvest and transplant techniques here in Australia,” said Martin who also has emailed Professor Peter Collignon about hygiene and hospital acquired disease.
“I have made sure I went to reputable sources,” said Martin, and this included information from the Leukaemia Foundation, including the information booklet, Myeloma – A Guide for people with myeloma, which they picked up at the hospital.
“It was very, very helpful, and helpful to us as a family,” said Patricia.
“We read it from cover to cover a couple of times.”
Martin has also attended myeloma support groups at the Leukaemia Foundation’s accommodation centre in Canberra and he volunteers, providing peer support and insights on his experiences with myeloma.
“I think it’s important for me, as someone who is a long-term survivor to be talking to people who are in the early stages of trying to cope with things,” said Martin.
One of his key pieces of advice is understanding that “myeloma is an individual disease”.
“The way in which you respond to the various treatments is going to be different for everyone.”
And his take home message is, “keep on keeping on”.

Support means “you don’t have to do it alone”
Patricia said her GP had to “bully me” to get help from the carers’ association when she needed it.
“We were brought up to be very independent and not to ask for help. But people are keen to help, to bring casseroles and to work in your garden when you’re too sick to do it. And you’ve got to learn to say, ‘yes, thank you’,” she said.
“If you can get that sort of help, it’s for your own piece of mind and is a way you can manage this disease, but it’s also support for your family,” added Martin.
“We needed a bereavement counsellor when we lost Martin’s brother, and when we thought we were going to lose Martin, and when the cat got a tumour and had to be put down,” said Patricia.
“I mean, it’s all a bit much. And when Martin was having terrible steroid rages with dexamethasone, the carers’ association and Leukaemia Foundation helped us cope with the effects on the family of some aspects of treatment.
“I guess a big message is you don’t have to do it alone,” said Martin.
“There are all sorts of community organisations that can help as well as family and friends.”
Need support? Please connect with our Blood Cancer Support Coordinators on 1800 620 420 if you need to talk, or to discuss how we can assist you with practical support. Alternatively, you may prefer to fill out our online referral form for us to reach out to you https://www.leukaemia.org.au/information-and-support-service-referral/
* A combination of vincristine, doxorubicin, and dexamethasone.
Last updated on October 24th, 2022
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.