ET or PV? That’s the question Sue’s been pondering for years
Since her diagnosis with essential thrombocythaemia (ET) in 2013, Sue Taylor has been curious about whether she may in fact have a different type of MPN–polycythaemia vera (PV).
“It certainly was always at the back of my mind,” said Sue, 64, of Sydney.

Her search for the answer has seen her change her treating haematologist several times and go overseas to an MPN conference, so she could put the question to international experts.
Sue’s main interest in having an accurate diagnosis centred around her risk of thrombosis (blood clot) but was also about possible future access to new treatments and clinical trials
In 2009, soon after Sue took a voluntary redundancy from her sedentary but stressful job in the Australian Public Service, she got “some strange visual symptoms” which “was a bit concerning”.
When an ophthalmologist couldn’t find anything wrong, Sue put these episodes down to “just something happening” and got on with life, despite increasing episodes. (Later, Sue found out she had scintillating scotoma)
Sue and her husband, John, have spent much of their lives together working overseas and travelling extensively, especially after her retirement.
“We’ve packed a lot into our life, and it has been wonderful,” said Sue.
“We were in a fortunate position to be able to take a bit of time for us, while fit and healthy, to enjoy some time together doing things we wanted to do. For us that meant a lot of travelling.
“Having three close family members pass away in the recent past made us think you can’t take anything for granted.”
Four years on, when Sue went to her GP, a routine blood test showed her platelets were “fairly elevated” and, looking back at previous years’ blood results, it was apparent that although in the normal range, her platelet count had been increasing.
“At this point I was sent off to a haematologist and had the JAK2 test. It was positive and I was diagnosed with ET.”
“I felt very well and would never have thought I had anything wrong with me,” said Sue, then aged 53.
“Honestly, it’s a shock when you’re first diagnosed, but I was reasonably philosophical and just grateful it wasn’t something worse. I’d recently seen my dad go through motor neurone disease.”

Her haematologist didn’t seem to think her visual symptoms were significant but put her on baby aspirin due to her high platelet count.
“The amazing thing, which I didn’t realise until a year later, was… I never had another of those episodes… except once, when I went off aspirin before having surgery.”
Being “an extremely curious person” and studying genetics for her science degree at uni, Sue had “done a bit of reading” on the internet about MPN before seeing her haematologist.
“I was told there was nothing to worry about but if my platelets continued above 600, then he might think about putting me onto hydroxyurea.
“When I asked about a bone marrow biopsy he said, ‘you don’t need to know about that yet’, which was like a red rag to a bull. He really wasn’t the right haematologist for me.
“I’m a very research and evidence-based sort of person, so I tried to see someone who was into research and preferably had an interest in MPN.
“I was fortunate to be linked up to a really special haematologist, who was involved in research, but MPN wasn’t his thing,” said Sue.
“Then I read about this third person who had an interest in PV and had been involved with PV study groups earlier in his career.
“I was referred to him, which was alright until he retired.
“He’d written a paper on platelet-mediated visual disturbances and was the first person who actually thought my visual disturbances might have some relationship to my ET. He was a bit excited because he thought I was a classic case.
“In the meantime, I did more reading and learnt a lot. I discovered MPNs are quite rare, there wasn’t a lot of research being done, certainly not in Sydney that I could find,” said Sue.
She came across an Italian research paper about JAK2 and PV.
“They worked out that a haematocrit–a measure of the volume of red cells in your blood–of 45 or below was the range for people with PV, to avoid a thrombosis which is the main immediate concern of haematologists treating MPNs.
“Although I’d been diagnosed with ET, I was very curious about this because my haematocrit was regularly measured at 47-48. I was concerned I was at risk of thrombosis, having a haematocrit that high.
“The JAK2 mutation was only discovered in 2005 and there were debates and different points of view about whether ET and PV were different diseases.
“There’s been research which shows a lot of people have been incorrectly diagnosed with ET who actually have PV,” explained Sue.
“I wondered if I had ‘masked PV’; a type of PV where you don’t quite fit the criteria to be diagnosed with PV, in terms of your blood counts, but it can be masked because of very low iron levels in your blood.
“I had very low iron levels, but I really couldn’t get any haematologist to be terribly interested in that. They were always interested in my platelets, but not my haematocrit.”
In 2017 Sue went to a patient conference, held by the MPN Education Foundation every two years in the U.S., that brings together eminent MPN researchers and clinicians from around the world.
“It was a fantastic experience. I met some of the MPN patient representatives in the U.S., and other patients.
“I still didn’t really get my question answered but I was told that, to be on the safe side, I should make sure my haematocrit was lower.”
Sue heard about pegylated interferon alfa-2a (Pegasys®) at the conference, and that in some cases it can lead to molecular remission.
“In Australia, haematologists were only talking about hydroxyurea, which I was concerned about taking because it exacerbated non-melanoma skin cancers, and I have very fair skin.
Sue had been on watch and wait and her only treatment was aspirin, until 2016, when she started having “funny spells”, didn’t feel very well, and her blood pressure was “a bit up and down”.
“I agreed reluctantly to go on hydroxyurea, just to get my blood counts down and to see if that made any difference,” said Sue.
“My understanding was that hydroxyurea could be quite good for controlling your blood counts, but it didn’t do anything about controlling possible disease progression to two other versions of MPN–very active PV and myelofibrosis (MF).
“One thing MPN patients are very interested in is the risk of disease progression and how they might minimise that.”
“It’s only a low risk but it’s there, and there’s really no way of predicting who will progress. There’s still a lot that’s unknown.
“I was always very interested in interferon but any haematologists I spoke to in Australia at that time said the side-effects were difficult, and ‘you don’t want to be on it’.
“I was aware pegylated interferon was available in Australia on compassionate grounds, and knew efforts were being made to try and get it on to the Pharmaceutical Benefits Scheme (PBS).
“At the time it was about $1400 a month… more than I wanted to pay.
“I was really grateful when Nathalie Cook (a MPN patient and advocate) was successful in her effort to get Pegasys on the PBS and I thought, ‘yes, I’d really like to give it a go’.
“As soon as it became available, I asked my haematologist to put me on it and I had to be assertive in my request. I was her first patient on it for MPN,” said Sue who had been on hydroxyurea for 18 months.
“Once I went on Pegasys, I was extremely relieved and surprised. I don’t think I’ve had any side effects and I haven’t had any headaches,” said Sue.
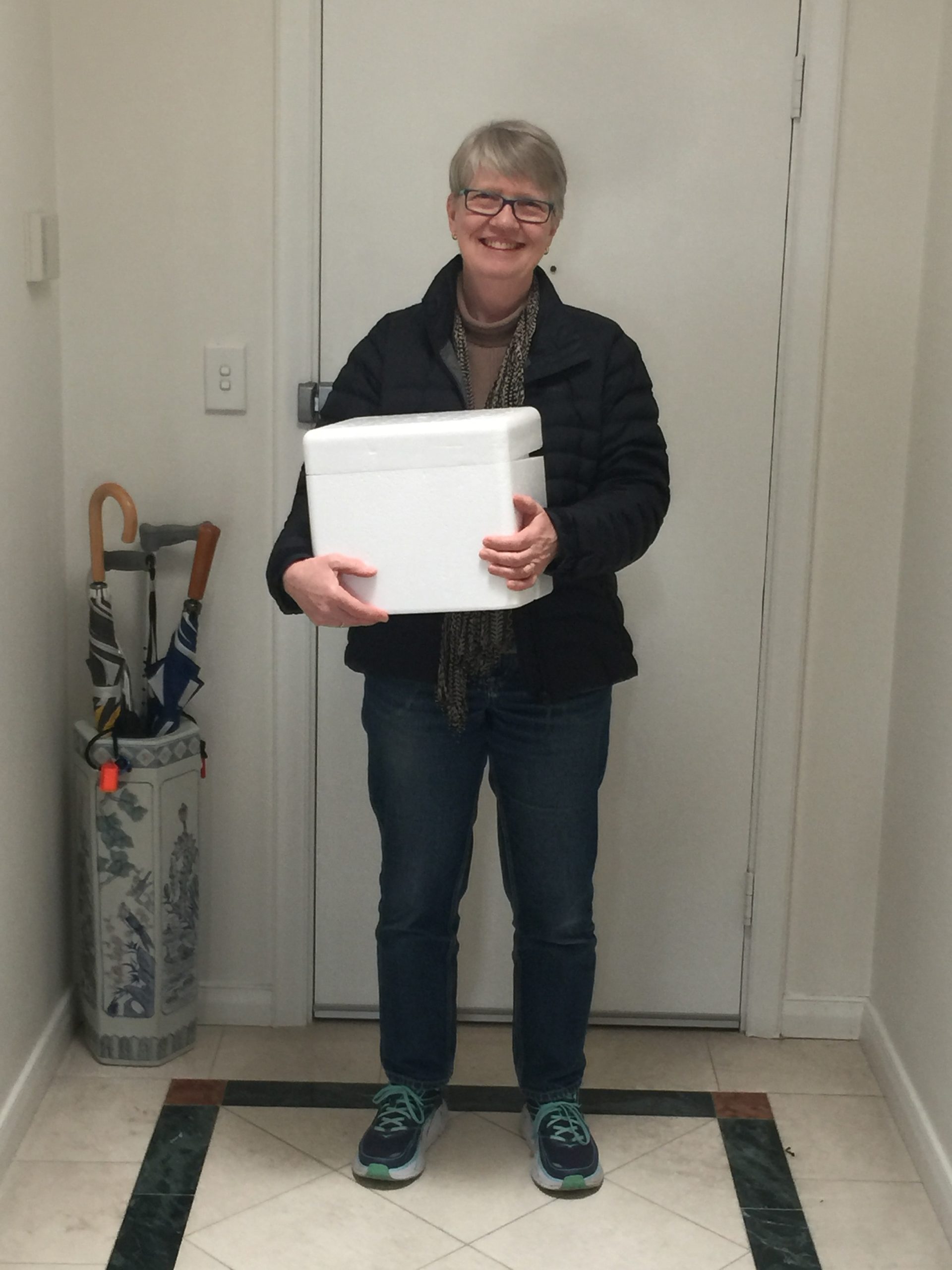
“It takes a bit of getting used to, injecting yourself, and I got advice and tips from other patients that was very helpful.
“I was able to live my normal life. It really didn’t impact me. And I feel incredibly grateful for that.
“In my case, it worked very effectively at a very small dose and I’ve actually been able to halve the dose. So, I only use it every fortnight and I’m trucking along quite well.

“My bloods are all within normal range.
“I don’t want to sound as though I’m an advocate for it, because everybody’s got their own response to different treatments, but for me, it’s worked well so far.”
Sue’s been on Pegasys for more than two years. This includes a four-month break when she “had an episode” and ended up in hospital with a high fever and severe chest pain.
“We’re not sure if that was related to the Pegasys or not, but I’ve been back on it again for a year and it hasn’t happened again.
“In the course of that, I sought another opinion from a haematologist with more experience with interferon, and other medical specialists.
“I was very well looked after, and my current haematologist was very good at facilitating all that too.”
“And that haematologist, who I saw for a second opinion, looked over my full history and was suspicious that I may well have masked PV, which was interesting.
“I still have the diagnosis of ET formally but I’m not so worried about it now, so long as I’m on a drug that is keeping my haematocrit under control.”
“My haematocrit has been below 45 since I’ve been on treatment so at least I feel comfortable that any thrombosis risk is being managed.
“The other reason I was really keen to have an accurate diagnosis was that when new drugs come along or clinical trials, they usually have pretty specific criteria as to who can have them,” said Sue.
“Who knows what might come along in the future.
“There are some really positive results coming out of clinical trials into a new type of interferon alfa-2b, called ropeginterferon (Besremi®). It’s a slightly different formulation and is longer acting.
“It’s been tested on people with PV, and the results have been quite good as reported at ASH [the American Society of Hematology annual meeting] and in Europe at some haematological conferences.

Sue feels very fortunate her MPN hasn’t held her back in life “at all”. Her response to this “strange diagnosis” was to focus on having a healthy life and doing as well as she could by eating healthy food and controlling her weight.
She was already doing pilates and bushwalking, so she joined a gym and went several times a week for her cardio fitness.
“The joy of using your body and feeling strong and fit I found to be an unexpected benefit… a buzz. I felt really good,” said Sue, but she developed an ankle problem which has taken “some years” to get better, with “months and months” of rest.
“I’ve got severe arthritis in my ankle. That’s probably the worst thing that’s happened to me.
“It’s the inability to do what I love most, which is being physically active.
“I still do pilates and walk, but only on the flat,” said Sue who is careful with her diet.
“I figured that if you’ve got an ankle injury or knees or hips, keeping your weight at a good level is a good thing, and it also helps with your mental wellbeing.
“I eat more of the good stuff and less of the not-so-good stuff” said Sue.
That means more good carbs, vegetables and fruit, fish, small portions of meat, more beans, nuts and seeds, and not eating between meals. She still treats herself to a slice of birthday cake and dark chocolate, going for quality not quantity.

Sue tends to think of MPN “as a chronic condition, like diabetes”.
“I’m focusing on doing what I can to maintain my general health and fitness.”
“People can be worried by MPNs being called ‘cancer’, which has the unfortunate effect of frightening people. I can understand why it’s called a cancer, but there are benefits for MPNs to be cancer, including cancer funding and getting more notice from doctors and researchers.
“I have never felt frightened of my diagnosis. My intellectual curiosity to find out more about MPNs is my way of taking control.
“I was given no information,” said Sue about when she was diagnosed.
“When I moved to my second haematologist and was in the waiting room of a big teaching hospital in Sydney, I found all the Leukaemia Foundation booklets. I was very excited to see the MPN one amongst the others. It gave me some basic information.”
Travelling is not so high on Sue’s agenda these days. She’s providing support to her elderly mother and has two grandchildren to enjoy time with, and one on the way.
“We’re a pretty close family, so we like to see as much of them as we can,” she said.
Looking back on her journey with MPN, Sue has realised it “takes time to adjust”. From her interaction with other MPN patients, she understands that everyone has a different experience with their MPN, and there is no “one size fits all.”
Last updated on March 4th, 2021
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.