Expert Series: Prof. Wendy Erber – a tool predicting the potential progression of MPNs coming soon
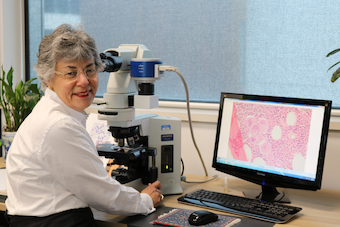
Professor Wendy Erber and her research team in Western Australia are developing a monitoring tool they hope will identify MPN patients who will go on to develop leukaemia.
This world-first blood test, expected to be available clinically in a couple of years, takes a “totally different approach” to looking for cells with abnormal chromosomes.
And it will be game-changing for people with MPN because currently nobody can predict the risk of their disease becoming serious, transforming to acute leukaemia or if their bone marrow might stop functioning.
“This is really new technology, which is taking chromosome testing to the next level because it is so much more sensitive and specific than other chromosome tests available,” said Prof. Erber, Professor of Pathology and Laboratory Medicine at the University of Western Australia, a diagnostic haematologist at PathWest, WA’s state pathology facility, and a member of the Blood Cancer Taskforce.
In 2018, Prof. Erber received a Eureka Prize* for Innovative Use of Technology for Immuno-flowFISH – the method she invented with two other members of her research team. It can identify a change in the tempo of diseases, including MPN, heralding the need for further investigation or to start a new therapy or the next round of therapy, leading to better outcomes.
Research on this discovery has been published and has received “great interest” by research centres around the world. The Immuno-flowFISH method has been patented, ongoing research work is refining the technique so it can be standardized and interpreted, and a study is about to start.
“It’s not at the stage yet of being an accredited test with a Medicare item number – it’s still very much in the development phase,” said Prof Erber.
However, the instrument that is needed to do this test is available in every state of Australia and her aim is for the test to be clinically available to all MPN patients and other cancer patients too.
From Sydney to Oxford, back to Sydney, over to Perth, on to Cambridge, then back to Perth
The development of this technique, which Prof. Erber describes as a “predictor of progression”, is a major achievement in a remarkable career driven by an overriding interest in new discoveries.
After graduating from medicine at Sydney University, as a junior doctor with an interest in surgery, Wendy realised that “cutting out a lesion wasn’t going to cure people… we needed to better understand the underlying pathological process”, she said.
And the reason for developing an interest in the haematological malignances was deeply personal – her younger sister, Jeannette, was diagnosed with and died from acute myeloid leukaemia (AML).
Winning a Rhodes Scholarship gave Wendy the opportunity to go to Oxford to study, and during her four years there she worked “with David Mason, one of the best clinician scientists in haematology in the UK, who was developing new techniques in diagnosing blood cancers”.
“I struggled to leave [Oxford] because it is just such a wonderful place, with some people with brilliant minds doing remarkable work, but I realised I needed to find my own career,” said Prof. Erber, and that meant training in haematology.
She returned to Sydney and, rather than treating blood cancer patients, Wendy chose to focus on the pathology of blood diseases, one of two components to haematology.
“One is a specialist doctor who treats patients with blood diseases, be they genetic, inherited, acquired, malignant or non-malignant. The other is the diagnostic arm, which is best explained as being a pathologist of blood and bone marrow, which is the blood factory, and which I look at under the microscope and make a diagnosis.
“The microscope, what the cells looked like and their biological basis, was where my interest was.”
“I got my ticket as a haematologist, then took a consultant job at the Royal Perth Hospital in diagnostic hematology, which was a big move,” said Prof. Erber.
“Perth is a lovely place to live. It’s very different academically from the other capital cities in Australia but I was still able to practice the type of haematology I wanted to do.”
After meeting her husband, also a pathologist (now retired), the couple had the opportunity to go to Cambridge to live and work at the university teaching hospital, where Wendy spent “seven fabulous years” working with Professor Tony Green.
“He was one of the few people in the UK, or even the world at the time, with an interest in myeloproliferative neoplasms,” said Prof. Erber.

“He was conducting the PT1 clinical trial in essential thrombocythaemia (ET). My role was ‘Wendy at the microscope’, reviewing the bone marrow pathology of patients with MPNs and correlating the morphological appearances with the genetics of the disease.
“When I first arrived in 2003, we didn’t know much about the genetics of MPNs.”
“I was fortunate to be on the team with Tony’s group and one of four groups that identified the specific mutation that occurred in most patients with MPNs. We then developed a diagnostic test.
“Not only did we identify the JAK2 V617F mutation, I was also part of the group that identified a second mutation in JAK2 in exon 12, which is very uncommon,” said Prof. Erber, who admitted to being “pretty chuffed” and “very proud” of her contribution.
“When I looked at the bone marrow of patients with a high haemoglobin who had polycythaemia but didn’t have the JAK2 V617F mutation, I could see under the microscope that, morphologically, some cases looked a bit different. From there, we were able to identify another mutation in JAK2, and it occurred in patients with this slightly different bone marrow appearance.
“It was an extremely exciting and productive time.”
“It took MPNs from being a group of disorders, the nature of which we didn’t understand, for which there were very few treatments available and very few people were interested in them, to now, where we have a blood test that we can use to help make a diagnosis and a range of different treatments that have been developed as a consequence of deciphering the genetic basis of the disease.”

Prof. Erber said the test for the JAK2 gene, which was first identified in 2005, “has now been ordered over 100,000 times in Australia”.
“I know that number through the Medicare funding and the number of tests that have been requested,” she said.
“For somebody with an unexplained high blood count, particularly an increased number of red blood cells leading to a high haemoglobin or a high platelet count, if there is no other obvious cause, then a GP would ask for this test, which is code for… is there a mutation in the JAK2 gene?
“That’s what we’re testing for and if that comes back positive then that tells us that it’s extremely likely that the abnormal blood count will be due to that genetic abnormality,” said Prof. Erber.
“Of people with an increased red cell count and high haemoglobin, 98% would have a JAK2 mutation, and around 70% of people with an unexplained high platelet count would have a JAK2 mutation.
“We have since learned there are other genes that can have mutations when you have a high platelet count, so if a JAK2 test is negative, it’s common for patients to be referred to a haematologist to do the further workup and determine the need to test for other mutations that are less common but do occur in MPNs with high platelet counts.”
Wendy returned to Perth in 2011 to take up her current professorial position at the University of Western Australia and also joined PathWest as a diagnostic haematologist with a focus on haematological malignances including the MPNs.
“My main task is reporting bone marrow tests**. When a patient has a bone marrow test done to investigate why they have an abnormal blood count, I look at the bone marrow under the microscope. The other main component is flow cytometry reporting – a sophisticated test modality that’s used to classify blood cancers.
“And on the university front, I teach science students, medical students, supervise Honours and PhD students, and undertake research.
About the myeloproliferative neoplasms (MPNs)

Around 1000 new cases of MPN are diagnosed in Australia each year and right now around 30,000 Australians are living with a myeloproliferative neoplasm.
“It’s a rare disease in that relatively few cases are diagnosed annually, but a lot of people are living with an MPN,” said Prof. Erber.
She describes the MPNs as “a group of malignant diseases where the bone marrow is making too much blood uncontrollably”, and uses a car analogy, where “the accelerator is stuck down and the car is driving forward autonomously”.
“The bone marrow is in overdrive, making blood continuously without the normal checks and balances,” she explained.
“We know these are blood cancers because a genetic change has occurred in the bone marrow cells during the person’s life; they weren’t born with it.”
And this genetic change has put the bone marrow into a continuous phase of making too much blood.
“It can make too many red blood cells, too many platelets, and sometimes, in some patients, too many white blood cells as well,” Prof. Erber said.
“Sadly, in most cases, we don’t know the cause. We know the genetic basis, we know the biology, but we don’t know why it has occurred, although a very few cases may be a result of tobacco, and there are a very few cases where there’s been a family history of the disease.
“If we knew the underlying cause, then we would tell people not to undertake certain behaviours or to not be in certain environments.”
The risks of having an MPN
The greatest risk for people with an MPN is a bleeding or clotting problem.
“They could have a heart attack or stroke or they could bleed, because the platelets – even though they’re often increased in number – don’t work normally. They may be overactive, leading to clotting or underactive, leading to bleeding,” said Prof Erber.
“The treatments we give are to try and control the number of platelets and can also affect their function.
“We have to make sure people’s red blood cell counts and platelet counts are kept under control, throughout their life, but we’re not curing them, we’re just controlling any clinical effects.”
People with MPN also are at risk of their disease changing.
“The disease can transform to acute leukaemia or progress to the bone marrow becoming scarred and no longer able to make blood, which is odd,” commented Prof. Erber.
“They’ve gone from their bone marrow overproducing and making too much blood uncontrollably, to burning out and being unable to make blood anymore and the bone marrow becomes fibrotic; full of fibres that are like scaffolding.
“The greatest concern for patients is… they don’t know if either of those two things will happen. Will they get acute leukaemia or will their bone marrow stop working altogether, and if so, when will it happen?”
“We can’t tell them,” Prof. Erber said.
“The only way of knowing if things are going awry is with regular blood tests which may include testing for new genetic abnormalities – new mutations in the DNA.
“We see patients once every six months or once a year or however often their haematologist thinks necessary.
“We do a blood count and examine the patient to see if there’s been any increase in the size of the spleen, which can indicate that the disease is changing.”
Prof. Erber said up to one in five patients will have changes and these occur over years.
“A patient rang me in a flap some years ago. She was really concerned. She had been told she had an MPN and that in 10 years the disease was likely to change and progress to something nasty; AML or fibrosis. And, she said, ‘today is the day. Today is the 10-year anniversary and I’m worried’.”
However, “it’s not quite that scientific”, said Prof. Erber.
“It may or may not happen, and it may happen at two years, five years, 10 years [post diagnosis].
“For most patients, it’s many years after the initial diagnosis, but even then, it’s not everybody – it’s up to about 20% of them, and that’s why you don’t transplant everybody up front.”
While a bone marrow transplant is the only curative therapy for MPN, it is not necessary for the vast majority of patients because at least 80% of them will “live long lives”, said Prof. Erber.
“People are living together with their MPN and they may have a normal lifespan.”
“It’s only when we identify changes in the blood counts and clinical features that we might say, “the only way we can potentially cure you is with a bone marrow transplant, but a transplant is not without its own risks and is only suitable for people under 65-70 years of age.
“That’s the biggest challenge for researchers – finding a cure for MPN.”
And that’s the greatest unmet need for people diagnosed and living with this rare blood cancer.
The importance of a bone marrow biopsy at diagnosis
“A lot of hematologists think if you’ve got somebody with a high blood count and you do a JAK2 test that comes back positive – that’s all you need to do to make a diagnosis,” said Prof. Erber.
“My view is that patients should have a bone marrow test when they are first diagnosed.”
“That gives me or my colleagues an opportunity to look at the bone marrow and get a very accurate description of what it looks like at diagnosis – a baseline.
“Then, if things do change over time – clinically or on blood testing – and if we do need to do another bone marrow test when the patient is not feeling great, we can compare that bone marrow with the original appearance.
“That’s when we can see if there has been a change,” said Prof. Erber.
“The World Health Organization agrees, or I agree with them, that patients should have a bone marrow test at diagnosis, to be certain of the MPN subtype, and as a baseline for future reference.”
And if you don’t do a bone marrow test, then you are not entered into the cancer database as having an MPN, said Prof. Erber.
“There’s great variation in this practice by clinical haematologists, great variation,” emphasised Prof. Erber, who, along with Dr Cecily Forsyth, a haematologist at Gosford, north of Sydney, and others, authored an article about the prevalence of MPNs in Australia that was published in the Royal College of Physicians Internal Medicine Journal in 2021.
It highlighted a “marked variation” in the reported incidence of MPN, not only between states but also between regions with similar demographics, which was attributed to a variation in the practice of performing bone marrow biopsies at diagnosis.
“The variation in prevalence is probably not real but due, in some places, to some haematologists not doing bone marrow tests,” said Prof. Erber.
“And that’s really important, to work out incidence – the actual reality of how many people there are in Australia with these diseases.
“We believe there is under-reporting [of MPNs] in Australia because not all patients are having a bone marrow test.”
Using a new tool that looked at cancer diagnosis and colour coded a map of Australia based on the prevalence of disease, Prof. Erber said Gosford looked like a hotspot for MPNs compared to Sydney.
“But it was because Cecily was doing bone marrow tests and haematologists in the city weren’t.”
Professor Erber’s medical research on predicting disease progression
Professor Erber’s longstanding interest in the appearance of patients with myelofibrosis (MF) – “this end-stage burnout phase” of the disease – dates back to her time in Cambridge when she began looking at the bone marrow of MPNs down the microscope.
“It [MF] is very different from the more chronic early phases of polycythaemia vera (PV) or essential thrombocythaemia,” she explained.
“There are a number of appearances that I can see under the microscope that are quite different, particularly with one of the cells, called the megakaryocyte, which starts to look very bizarre.
“It’s a big cell with a very long name, ‘mega’ meaning big.
“I’ve been interested in what is it about the megakaryocyte and its relationship with this progression to myelofibrosis?
“We’ve been looking at the genetics of megakaryocytes, which is a very challenging task, and more recently looking at platelets, which are generally increased in number in MPNs and are made by these megakaryocytes.
“And we’ve been looking at the genes that are being expressed within those platelets and finding that they’re different in MPNs from normal platelets, and in myelofibrosis, they’re different from ET and PV.
“What we’re trying to determine is… could we use regular blood testing, looking at those genes and their expression in platelets, as an indicator that the disease is about to turn and progress from PV or ET to myelofibrosis?
“We’ve also started looking at platelets in AML as well, because if there is a change in the genes in platelets going from this chronic PV and ET phase into the aggressive leukaemia or fibrosis phases, then patients who are an appropriate age could potentially proceed to a transplant, knowing that we have identified this progression before it manifested clinically (before the person actually gets sick).
“In effect, the research is trying to develop a predictive model of progression using platelets.”
“We may not know whether the patient would progress to AML or to myelofibrosis, but we’ll be able to say that there is a change that is indicating the disease is progressing to something nasty, and that may then lead to other tests.
“Our hypothesis would be that if we can identify that progression earlier, then the patient could go to transplant earlier before they’re really unwell. That would lead to better outcomes.
“And it’s only when we identify some of these changes that we might then say, ‘the only way that we can cure you is to do a bone marrow transplant’.
“Early data shows there is a difference in the genes that are expressed by platelets between patients with ET and PV, compared with MF.
“What we need to do now is to monitor patients over time, testing their blood regularly, to see any drift or changes, realising of course that progression may occur 20 or 30 years later.
“And it could be that the changes we’re seeing are due to the treatment they’re on, so we need to do more follow-up testing of patients.
“It’s still a hypothesis, and it always takes longer than we would like, but in two to five years we hope to have some answers.”
More about Immuno-flowFISH
Many patients with MPNs have abnormal chromosomes and standard chromosome or cytogenetic tests are “manual and quite labour-intensive”, said Prof. Erber.
“One looks at just 20 cells of the millions and millions of leukaemia cells in a person’s body when they’re first diagnosed, and another one, called FISH, which stands for something complicated, looks at 200 cells,” she said.
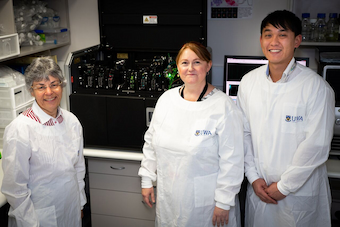
Prof. Erber, Dr Kathryn Fuller, “my right hand in the scientific wet lab” and Henry Hui, who was a PhD student at the time, invented Immuno-flowFISH – an imaging flow cytometry method that uses “an instrument which can test a lot of cells (up to 10,000 times more cells than current tests) in a short period of time”.
“We look at the biological characteristics of the cell – the various biological markers or blood groups on the outside of the leukaemia cell and that way we can be absolutely certain we’re looking at the leukaemia because we’re looking at features of a leukaemia cell.
“That’s the immuno component, and at the same time, on the same cells, we’re doing FISH which is the chromosome test which probes the nucleus of the cell.
“We can get down to detecting one leukaemic cell with the abnormal chromosome in 10,000 background normal cells, which is incredibly powerful and very accurate.”
“What we’re about to do is to look at the blood of patients with MPNs and see if there are any cells in their blood that have abnormal chromosomes.
“One of them is chromosome number 17 where we know there’s a very dangerous gene that can be lost and that can result in acute myeloid leukemia appearing.
“It’s another blood test that we’re developing as a monitoring tool to be able to identify MPN patients before they get really florid leukemia.
“We’re looking at leukaemia through a new lens – looking for these changes in the chromosomes of a cell using a totally different approach.
“Instead of looking at 20 or 200 cells, we’re looking at 10,000 or 20,000 cells. We can identify one leukaemia cell with the abnormal chromosome in 10,000 background normal cells.
“With the power of this technique, we’re identifying a needle in a haystack.
“We might be able to identify that very rare cell that has come out of the blood and is telling us that things are about to go bad.”
Dr Hui is still working in Prof. Erber’s lab, refining and standardising the method and there are now three PhD students, two Honours students and two full-time scientists working on this project.
“It’s a really big part of my life,” said Prof. Erber.
“We’re not using it diagnostically yet. We’re got ethics approval and are inviting patients to participate in clinical research study.
“Most patients are very interested and willing even though they know it may not help them. They know that by supporting our research, it may well help the next person who finds themselves in a similar situation.”
Prof. Erber is also working with the MD Anderson Cancer Center, the largest cancer centre in the U.S. and is about to start a study with the Roswell Park Cancer Center in upstate New York.
This method potentially can be used for any cancer cell where there is a chromosome abnormality and where these cells escape from the primary tumour site and go into the blood.
“We started with CLL, the most common blood cancer in Australia and have done some work on myeloma, the second most common blood cancer. We have also done some work on the paediatric leukaemias, yet to be published, are now starting on MPNs and will soon commence a project on AML.”
Being on the Blood Cancer Taskforce
Professor Erber is the most recent member of the Blood Cancer Taskforce.
“I was very excited to be invited to contribute to blood cancers for patients through the Taskforce,” she said.
“It meant a lot to me that people recognise that I have contributed something over my career. I am honoured to be part of a really strong team that has been put together to assist government.
“We need to be better at what we do to improve outcomes, and it needs to be on a national basis.
“The initial report that went to government really made people aware of blood cancers, how common they are and that they’re going to increase in prevalence over the coming 10-15 years to become one of the most common cancer types in Australia.
“In particular it made government aware of the importance of this group of diseases that affects people at all stages of life,” said Prof. Erber.
“We need to ensure that government will work with the report [the National Strategic Action Plan] so the recommendations are acted on in a timely fashion.
“A lot of new therapies are available. We must make them accessible and make sure we’re giving those new treatments to the right people.
“Some of the work we are doing with Immuno-flowFISH and with the MPNs feeds into that by refining the diagnosis. Making sure we get it absolutely spot on will then enable us to choose the best treatment.
“Data in the Taskforce document, and which has been reported in other parts of the world, is that there is a diagnostic error rate of 25%, which is quite high.
“It doesn’t mean we actually get it wrong, it’s just we don’t get it sufficiently right. What I mean by that is we need to get right down to the genetic level to make sure we get the really precise diagnosis because that will then determine the very best treatment for that person.
“It’s not one size fits all anymore. It’s that personalised approach that I think is really important.
“My sister died after five months with AML, in 1979. If she were diagnosed today, would things be different? Yes, they would because she would now have a host of genetic tests available to her. And based on the results of those, she would get better treatment, not just the same treatment that every other AML patient got. It would be personalised, based on the really precise biology of the leukaemia. And that’s what the Taskforce will deliver.”
* The Australian Museum Eureka Prizes are Australia’s leading science awards, rewarding excellence in the fields of research and innovation, leadership, science engagement and school science.
** A bone marrow test (bone marrow biopsy) involves removing a small sample of the bone marrow inside your bones for testing, to find the cause of problems with red blood cells, white blood cells or platelets. Bone marrow is a soft tissue in the centre of most large bones. It makes most of the body’s blood cells. The biopsy is done using a small needle inserted into the bone.
Last updated on January 3rd, 2023
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.