Dr Traver’s fascination with how leukaemia happens
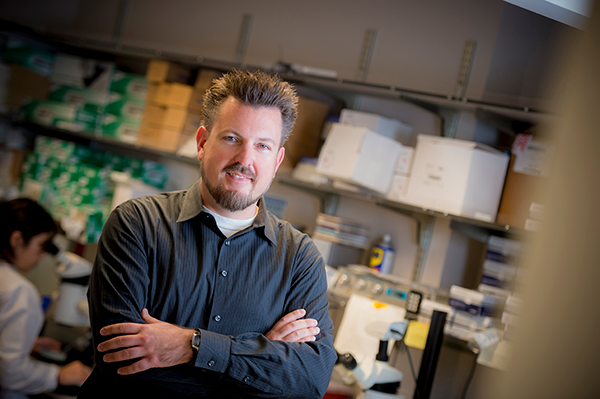
Dr David Traver is an experimental haematologist who specialises in haematopoiesis*. The Professor of Cellular and Molecular Medicine, and of Cell and Developmental Biology, at the University of California (San Diego, U.S.) spoke to AML News at the International Society of Experimental Hematology (ISEH) conference in Brisbane (Aug 2019), where he was awarded the Leukaemia Foundation-sponsored McCulloch and Till Award and gave the closing lecture on Decoding the molecular cues that regulate HSC specification.
How do you feel about receiving this award?
It was quite a surprise and an honour. This has always been my favourite meeting. I gave my first talk in science at this meeting when I was a graduate student, in Vancouver in 1997 or 1998. I was terrified. There were all of these big names in the audience who I had only read about as a third-year student. But everyone was so open and welcoming, and they were all very approachable. It has been my favourite meeting ever since.
And now you’re one of those famous people!
I guess [laughter] but I’ve never cared about being famous. I’d like to be rich, but I think I chose the wrong career for that. I generally don’t like to be the centre of attention, so I sometimes wonder why I chose this career. The idea of being the lab’s spokesperson was initially challenging for me, but I’ve learned over the years to enjoy it. I love the science and love to always be learning.
How did you become an experimental haematologist?
I joined the immunology program at Stanford University, where I had a choice of about 30 labs working on things related to immunology. I was attracted to Irv Weissman’s group because he was focused on haematopoiesis, meaning the study of how blood cells arise, how stem cells work, and how leukaemia happens. And those were the questions I found really fascinating, rather than classic immunology. I liked the process of blood formation, then became intrigued with development, genetics, and imaging, and fell in love with the zebrafish, which was an emerging system at the time.

What is your lab working on?
We are trying to understand how the stem cells that make the entire haematopoietic system are born. In other words, how they are first formed during development of the embryo. One of the big goals of regenerative medicine is to harness the technology of induced pluripotent stem cells [that have the potential to make all the cell types in our bodies], as discovered by Shinya Yamanaka, to make patient-specific blood cells. What we can’t do yet is make blood stem cells from this primitive precursor. A transplant for a person with leukaemia or a blood-based disease needs haematopoietic stem cells (HSCs), to provide lifelong regeneration of the lineages they need. Ultimately, the goal for many of us in the field is to try and take these human pluripotent stem cells and instruct them to generate HSCs. Despite attempts for 30 years, we’ve never been able to do it because we don’t yet know enough about how the embryo does it.
What are your big picture goals?
One is to understand how the embryo makes HSCs. That’s why we use zebrafish. They are born externally from their mother and are completely translucent for the first week of life. They develop into a free-swimming animal with a beating heart and stem cells within 24 hours of fertilisation. We can use fluorescent transgenes to light up the HSCs to watch how they behave inside a living animal in real time.
“We saw the HSCs being born out of one of the major blood vessels, just by watching to see what happened.”
There were several theories about where HSCs were born in the embryo. We imaged animals with fluorescent blood vessels and fluorescent HSCs via a 24 hour time-lapse and the evidence was irrefutable. That is what we’ve been working to better understand ever since.
What does this finding mean?
Once we knew, finally, where stem cells were coming from, we could then work to figure out how, genetically, those cells were born… how they are made, how the environment instructs them what to become. What we are working on now is to target single HSCs at the site of emergence [where they are born] and activate a single oncogene** in a single stem cell.
“This is how everyone thinks cancer starts.”
You take one hit, probably to a stem cell because it has to live long enough to accumulate more mutations. We can ask, is that sufficient? It is not thought that one mutation is ever sufficient to cause cancer, but it might be sufficient to start the process.
What questions are you asking now?
If a clone we are working on does give risk to leukaemia later on, how does it do it?
We can pull out those clones and ask every week… how does that clone change in a molecular way? We can activate an oncogene in a single stem cell in a hundred different embryos and pull out 10 embryos every week or month and ask… how are they changing? This is the five-year plan; what we are working to do now. You can only do these amazing experiments in zebrafish because everything happens ex utero. This approach cannot be taken in mouse models because you can’t effectively target those stem cells that early.
“And the powerful thing is that we’ve all come from a common ancestor.”
So, the things that we discover in zebrafish are almost always applicable to studies in mice, frogs, or humans, since our immune systems have all derived from a shared ancestral source. The zebrafish we work on are really beautiful. They’re remarkable little creatures. You can see every cell in their bodies and how they behave in real time. My talk [at ISEH] includes a few time-lapse movies people in the lab generated. We do a lot of our early work, genetics, imaging and stem cell biology in the zebrafish, and revalidate our findings usually in the mouse embryo, where my early training was. Then often we take what we’ve learned and test it in human pluripotent cell systems. I think, ideally, if we can show the same thing is true in systems as different as fish, a rodent, and us, then it is fundamental and a great foundation to move forward.

How is your work contributing to blood cancer treatment?
We are studying the genetic mechanisms of how stem cells are born and how are they are maintained, and a big part of that is self-renewal. The hallmark of the stem cell is how it can make copies of itself forever, without becoming cancerous. Stem cells and cancer cells are the flipside of the same coin because cancer cells should never self-renew but somehow can. There could be a lot in common with the normal self-renewal mechanisms of stem cells and how cancer cells become transformed. Once we can generate these models of leukaemia starting with a single cell, we can do chemical screens and rapidly discover compounds that specifically kill that cancer.
For children with translocations in the mixed-lineage leukaemia (MLL) gene there is no effective treatment and it [MLL] is invariably fatal. It is thought that these translocations happen very early in development, because if you find identical twins where one has the mutation, the other almost always does too – meaning it happened very early in development, when each shared a circulatory system. So, this particular translocation is intimately involved in HSC emergence. It happens very early, which is one reason we think if we can activate expression of the human oncogene in a single stem cell it may accurately model what happens in these children.
What happens in your lab day-to-day?
It depends on the day. We have lab meetings once a week, where my students and fellows present their work and receive feedback from myself and others in the lab. I like to have a lab of 10-12 people, that is my ideal size. We have a journal club where we talk about papers that are relevant to what we do. I meet individually with everyone for at least half an hour a week to talk about their projects, their results, and to troubleshoot. One of my main jobs is to facilitate – to know the bigger picture, and how the individual components connect. I teach a fair amount – classes in stem cell biology, and there are grant cycles that are never-ending. It usually takes a couple of submissions to land a grant these days. And there are lots of faculty meetings and different seminars to participate in each week. I don’t do much experimenting anymore, I’m too busy with writing, grants, travelling, teaching and everything else that comes with this often crazy job.

What advice can you offer people with a blood cancer like AML?
One thing to try and do is to stay on top of what’s developing. If you have a disease that is typically hard to treat, see what is out there in terms of trials, talk to your doctor, and talk to researchers. A lot of patient-specific immune therapy, like the CAR T-cells, have had amazing success. But it has only worked so far for a handful of cancers and leukaemias. The cancer immunotherapy field is moving fast.
“I lost my own mother to AML 10 years ago.”
It was very demoralising and disappointing to see her taken by something I felt I knew a lot about and should be able to understand. My mum had a perfect match for the bone marrow transplant, she just couldn’t handle the preparative regimen. Her body rejected the platelets that were transfused following the chemotherapy. I think we just still don’t know enough. The regimens used are very generic, and damages all systems in the body. We need to get better at finding regimens that are more specific for each disease type.
What is your holy grail?
I would love to contribute to the recipe on how to effectively build a blood stem cell from scratch. Then we can translate our findings, from our embryonic settings, to in vitro settings in human pluripotent stem cells. I think, in a couple of years, we and others in the field will figure it out… but I have thought that for a while [laughter]. In the second phase of my career I would love to contribute more directly to human health and to helping people, because what we do in basic science often takes a long time to find its way to helping patients.
*Haematopoietic stem cells (HSCs) are the stem cells that give rise to all blood and immune cells. This process is called haematopoiesis and occurs in the bone marrow, in the core of most bones.
**An oncogene is a gene that has the potential to cause cancer.
Last updated on May 5th, 2021
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.