In My Own Words: Patrick Griffin was told he had months to live after a third cancer diagnosis
My journey began in 2005 when I was diagnosed with chronic lymphocytic leukaemia (CLL).

I was 59, a managing director of an international luxury hotel company, and not willing to face my mortality.
I was fortunate that I had an annual health check, which discovered the CLL. Being rather cavalier and told no action was required but to wait and watch, I continued with life as if there was nothing wrong. And I listened to the comment of a friend, “if you must get cancer, this is the best one to have!”.
On this positive note I started out feeling there were others a lot worse off than me, and that with the continual advances in medicine there had to be something that would help to control the cancer. This has come to pass, and in the meantime, staying positive and cheerful was the finest medicine of all.
Then in 2008 I was also diagnosed with prostate cancer. After a radical prostatectomy and being told I was in remission, I was hopeful of convincing myself I was cured of that cancer, which has turned out to be true.
The CLL started becoming more active in 2011. Again, I treated it as a matter of mild concern but felt that, at the age of 65, it was time to retire. I moved to Thailand to fulfil a dream of building my own small luxury hotel on the banks of the Mekong River.
Every three months, I kept a check on my bloods, but after about 12 months I became seriously ill and was admitted at Bangkok’s leading hospital. As I had no health insurance, it was agreed that I should return to Australia, so I left Thailand and went to Perth, being the closest city, and it was fortunate I have a sister living there.

On arrival I went to the ICU at Sir Charles Gairdner Hospital, under the care of Dr Julie Crawford. It was September 2012, I was diagnosed with diffuse large B-cell non-Hodgkin lymphoma and the prognosis was not good – I was given eight months to live!
I had a lot of treatment, and the first six cycles of chemo included a spinal injection of methotrexate. Then, due to the headaches I was having in December that year, I had a scan which showed blood around the brain. It was a chronic subdural haematoma [one of the most common neurosurgical conditions] and I had bilateral burr hole drainage [a procedure where small holes are drilled in the skull to drain the haematoma].

At this time, given my prognosis, it was suggested that I consider a bucket list. And, as I listed things that friends who had sadly faced similar situations had selected, I realised just how fortunate I had been. Instead of a bucket list, I decided to write ‘the’ book – an autobiography – that many people think of doing, but rarely do, and this proved to be so cathartic.
Nine months later, in May 2013, the lymphoma was in remission. Obviously, the amazing treatment I received in the hands of Dr Crawford and her team must be given the credit. But more than this, I believe the writing down of all the wonderful memories of people, places, and events that I had been fortunate to encounter in my life to date gave me such a positive feeling that this was not yet ‘the time’. There was still much to do, and this was confirmed by my recovery.

In December 2017 the CLL returned, and again Dr Crawford worked her magic with more chemo. I was admitted to hospital and started 1000mg infusions of obinutuzumab (Gazyva®). I went back into remission in April 2018… so life went on.
Unfortunately, in July 2020, the CLL again returned. I was treated with the oral drug, acalabrutinib 100mg (Calquence®) together with a cocktail of other drugs daily, and no chemo thankfully.
This treatment continues today and is ongoing indefinitely. I continue having a check-up every three months and my bloods are currently maintained as ‘normal’. I do feel tired and rather listless and have put on substantial weight, but at 77 this may be a case of age, and the surrounding problems of the COVID pandemic.

I am of the belief that still it is not my time and am enjoying life to the full. I have become far more aware of my mortality and am constantly reminded with a regimen of 14 pills a day. I also have sleep apnoea that involves the use of a continuous positive airway pressure (CPAP) machine. This combined with the side effects of the radical prostatectomy, results in numerous trips to the bathroom during the night, and a small level of incontinence does have an impact on any holiday or day away plans.
I do try to be the eternal optimist, but on occasions, especially when reminded of one’s mortality by friends (including Olivia Newton-John) and others you know ‘passing on’, one can experience a little depression.
I have always been a very open person and enjoy chatting, and as such have never been apprehensive about talking of personal issues and this has helped me – ‘a problem shared is a problem halved’. My family and friends have all been very supportive and talking of challenges in an optimistic way helps. I try never to complain or sound hard-done-by as people don’t want to continually hear a complainer. And in the same way, I avoid negative people who want to tell me of someone who had what I have and died!

I read scientific articles and medical updates about CLL. Back in 2005 my specialist gave me publications to read, and I’ve found other material myself around the cancer centres. When I was first diagnosed, I looked at the internet for information about CLL but found a lot of conflicting stories and they were not always positive, particularly around life expectancy, for example.
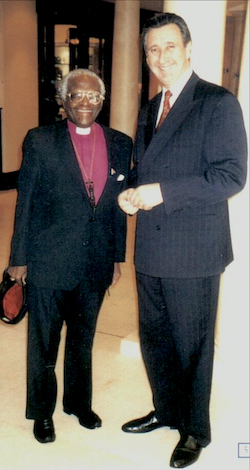
One thing that has been amazing in maintaining a positive and cheerful approach to life are the books* I wrote at the time when I was first seriously ill and at my lowest, dealing with a concerning prognosis. As mentioned, when considering a bucket list, I found that I had experienced such an exciting and fortunate life, I wrote it down. And as egotistical as this may sound, and I hope I will be forgiven if I admit that during times of challenge when I get the odd ‘down moment’, I actually read my own books just to remind myself of how lucky I have been and of the good fortune I have had.
Having had a career in luxury hotels, I enjoy travel, fine dining, and I try to maintain contact with the young people I have worked with. They are now older and more established, and I like to think I helped them along in their own careers.

Overall, I would summarise my experience with CLL as “irritating”, but I have not allowed it to be a major negative in doing what I want to do.
I fight to accept I’m getting older, and I am starting to struggle with the reality of closing in on 80, plus my medical and medicine issues. Travel is becoming more questionable. I had hoped to go to the UK to catch up with my elder brother with whom I was close, but he died in October. All my brothers have gone now and I’m next in line.
I want to stay around to care for and enjoy the happiness and companionship I have with my wife, Gan, who is younger than me and she keeps my mind young! I have been married three times and have a rather unusual family with six ‘international’ children who I spend time with. Seeing my eldest son marry last September and my younger son’s engagement are recent highlights.
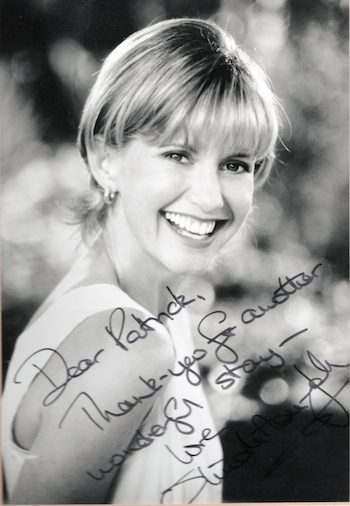
Along with my family, writing my books, which are now published and will be on some bookshelf somewhere forever, is what gives me the encouragement and inspiration to keep going on my journey with CLL.
When the pandemic began in 2020, we were just focused on our move from Western Australia back to Gosford in NSW, to be closer to our family in Sydney, and were more concerned about border closures. Being a rather isolated state, WA was also rather remote from the problems of COVID, and apart from the loo paper panic, there seemed little concern.
I have followed the government advice and, no longer being social animals, we did not go where the crowds were and always wore masks when shopping. I have had all the appropriate vaccinations and with precautions avoided contracting COVID-19 until late last year.
After Gan had tested positive on December 24, I tested positive with a rapid antigen test three days later. I immediately sought the antiviral drug that I had been advised to take within five days, in the event of a positive result. My haematologist instructed I take molnupiravir capsules in preference to the current drug as she felt that might have an effect on the cancer drugs I am taking.
COVID has affected me far worse than expected. I started the antiviral on December 30. At the time I felt OK but as the days progressed, I became short of breath and had a lot of coughing. On January 4 I went to Emergency at Concord Hospital and was put on oxygen and x-rayed. I was diagnosed with COVID-19 pneumonia and given dexamethasone. I also had immunoglobulin intravenously as per my haematologist due to having hypogammaglobulinaemia.
I was discharged on January 6 and had a negative RAT as of January 10. Since then, I have felt totally lethargic and at times so very tired. My breathing has improved but is still tight. I had not expected to feel so tired and hope this will improve although it seems to be a long process. It was suggested that I had ‘long COVID’ but this was not in the hospital discharge papers.
As I have faced each diagnosis and bout of treatment, I’ve felt a little more tired and less fit, not helped with the problems of aging. Overall, I feel I have coped well, albeit with a little more reality, such as getting my will in order and planning for what comes to us all… in time!
If you would like to talk to a Leukaemia Foundation blood cancer support coordinator or request support services, you can use our self-referral form at any time.
* The Grand Life is the title of Patrick’s trilogy. Parts I, II, III are available at: www.patrickgriffin.info