Diagnosed with leukaemia as a newborn
Zoe Li was a healthy baby when she was born in Perth in December 2017, but five weeks later her parents were told the shocking news… she had leukaemia.
By the time she had her second birthday, Zoe had been on a clinical trial, had gone to the U.S. for CAR T-cell therapy, and had a stem cell transplant in Sydney.

Now, Zoe is in remission, she goes to childcare like other healthy children, and this month she celebrates her fourth birthday.
Zoe’s acute lymphoblastic leukaemia diagnosis and attempts at remission
Her mum, Ping Hao said “it was really hard to believe” when her newborn daughter was diagnosed.
“I didn’t know children of such a young age could get leukaemia,” said Ping who’d had no complications during her pregnancy.
Zoe’s delivery was normal, and the results of blood and other tests, following her birth on 3 December 2017, were normal. But when Zoe was five weeks old, she had cold-like symptoms and stopped feeding.
“Because she was so young, I was a little bit worried, so I took her to the emergency department of our children’s hospital,” said Ping.

“They ran blood tests and found out that she had leukaemia.”
Zoe was diagnosed with infant pre-B acute lymphoblastic leukaemia on 8 January 2018. She was immediately admitted to the paediatric intensive care unit for an exchange transfusion to reduce her extremely elevated white blood cell count.
Just days later, Zoe started treatment on the Children’s Oncology Group’s AALL 15P1 study, an international clinical trial that had opened in March 2017 for infants less than a year old at diagnosis. But her disease was rising while she was on the study protocol.
“She became resistant to the chemotherapy and couldn’t reach remission,” said Ping.
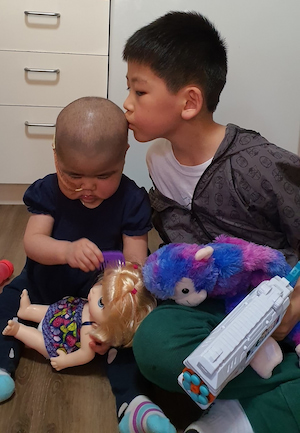
Zoe was withdrawn from the study after 10 months, and in December 2018 she began the first of two cycles of blinatumomab (Blincyto®) which was administered continuously via a pump, so she was able to be at home with her mum and dad, Jianqiao Li, and older brother, Vincent, who was five when his sister was born.

While the first round of blinatumomab did reduce her leukaemia load, Zoe wasn’t able to achieve remission from the second round of this treatment.
Next, on 26 March 2019, Zoe began a course of fludarabine-idarubicin (FLA-IDA) over five days. It was three weeks later that tests showed the treatment hadn’t worked. Zoe’s minimal residual disease had continued to rise.
“Basically, it did nothing,” summed up Ping.
“It was just really devastating. I mean, you have hope, drug after drug, that she could possibly reach remission, but it was just like everything, it just failed.”
“On the 16th of April they found out it didn’t work. We had this meeting with Dr Rishi who said basically they had run out of options for her.”
Zoe‘s haematologist, Dr Rishi Kotecha, said Zoe needed “CAR T-cell therapy to induce molecular remission”.
“The only option would be to have a CAR-T therapy in the U.S., because at that time, it’s not available in Australia,” said Ping, who by then had already started advocating for Zoe to access this treatment.
She knew of the CAR T-cell treatment option, from her membership of a Facebook group for parents of children diagnosed with infant leukaemia within the first year of life, called Infant Leukemia Support Group.
“We support each other and share information worldwide. There are parents from Europe and Asia but the majority are from the U.S. and they share information about which hospital to go to and provide contact details,” said Ping.
“I couldn’t find anybody in Perth who had the same disease as Zoe and was around the same age.
“When Dr Rishi said CAR T-cell therapy was the only option, I told him that I had made contact with two children’s hospitals in America.

“I’d reached out myself just after the FLA-IDA because I was afraid it wouldn’t work. I just couldn’t sit around and wait.”
“The hospital in Philadelphia didn’t respond fairly promptly, so we went to Seattle Children’s Hospital in the end.
“The cost of the CAR T-cell therapy is huge. It’s really expensive and my family couldn’t afford it.
“For all the treatment and the month in intensive care, it was around half a million U.S. dollars, and that’s not including accommodation and airfares.
“Dr Rishi applied for funding for us from the Australian government which paid for the treatment,” Ping explained.
Zoe’s CAR T-cell therapy
It took two months to arrange everything. Zoe and her mum and dad left Perth on June 16 and they spent the next three months in Seattle. Vincent stayed in Perth with his grandparents who had come out from China on long-term visas to support the family during this difficult time.

The day after their arrival the family went to the clinic to meet the medical team and Zoe was admitted, although they all stayed in accommodation near the hospital.
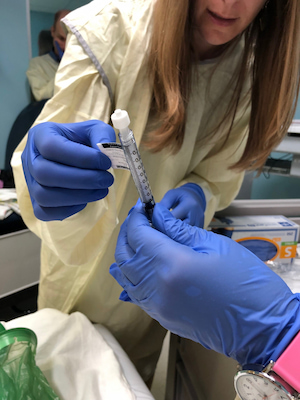
“They’re quite different to Australian hospitals. They send all the supplies to the place where we were living. We had to do the flushing and cleaning of Zoe’s central line.”
Zoe had a bone marrow exploration, “to see where the disease was at” and a week later her T-cells were harvested. Over the next five weeks Zoe’s T-cells were re-engineered; the chimeric antigen receptor (CAR) was inserted into the T-cells, then millions of the T-cells were grown in the laboratory.
During this time Zoe wasn’t on any treatment.
“Although she couldn’t reach remission, her leukaemia growth was really, really slow. We just waited for the T-cells to be ready,” said Ping.
“Zoe was quite well, so we were able to go around exploring Seattle for the time being, so it was really nice. We haven’t been to America before.
“She was 18 months old. She had just started to walk after we arrived in Seattle. She was a bit delayed as you can imagine.”
Jianqiao is an insurance broker, and he was able to work remotely from Seattle, “thanks to his employer; they were very understanding,” said Ping.
On 30 July 2019, Zoe’s T-cells were administered by infusion and she was closely monitored.
“They expect her to have a fever, and that shows the CAR T-cells are working, and she did have a fever on day three,” said Ping. “It was only mild fever and was she was admitted to hospital for about three days and was discharged.
“We didn’t really stay in the hospital. It was unexpected because I thought there was going to be a long hospital stay, but I think only for three or four days total,” said Ping, although they did go to the hospital regularly for Zoe to be checked.
“Unfortunately, the CAR T-cells didn’t work as expected, because if it is successful, she should reach remission 14 days after the CAR T-cell infusion, but she didn’t.

“The disease is still there, but it decreased. She was still not in remission.”
“Twenty-one days after the CAR-T cells, they did a bone marrow exploration, and she is still positive for the leukaemia cells,” said Ping.
“Dr Rishi sent me an email while we were still there, after we got the results, and he recommended Zoe have a bone marrow transplant.
“Although she couldn’t reach remission, it (CAR-T) reduced the disease to a level that she could have a bone marrow transplant.”
Zoe’s bone marrow transplant
On September 1, the family flew home to Perth and two weeks later, Ping, Zoe, and Vincent flew over to Sydney.
“Unfortunately, the Perth Children’s Hospital was not able to do the bone marrow transplant at that time. We did the transplant in Sydney Children’s Hospital, and Vincent attended the hospital school there,” said Ping.
“Luckily, my mum came from China to help and was able to stay with us at Ronald McDonald House in Sydney.
“My husband stayed in Perth due to his work commitments and visited us monthly. It is financially stressful and was a difficult time for him too,” said Ping.
None of Zoe’s family were a donor match, so she had donated cord blood cells “from a little boy who was an 8 out of 10 HLA match”. Her transplant was on 27 September 2019 after she had intensive chemotherapy.
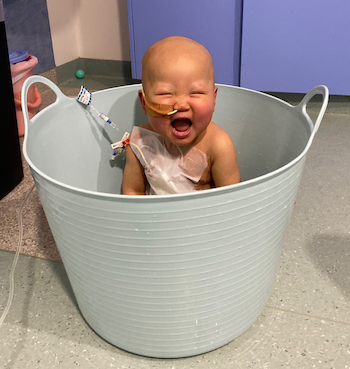
“It was really hard on her, so we need to stay in isolation for the whole time, which was really hard, but she did reach remission after the bone marrow transplant,” Ping explained.
“I couldn’t function before [the transplant], I was so worried, because I’m so afraid that it won’t work, like before.
“It finally worked. It was a really, really hard journey.”
After five months, the Li family returned to Perth on 1 February 2020. Zoe went back to the care of the Perth Children’s Hospital and was closely monitored with frequent bone marrow aspirations and blood tests.
“About 18 months later, she was still in remission,” said Ping.
“She is now lower risk, she stop all her medications and doesn’t need the bone marrow aspiration anymore. Her check-ups are every three months now.
“In five years, she’ll be cured.
“She’s really good and is almost four now. She attends pre-kindergarten and she’s been living a normal life.
“It’s taken me about two and a half years to finally settle back in Perth,” said Ping.
She was a logistics clerk prior to Zoe’s diagnosis and treatment, and had to resign, but Ping is planning to return to work in 2022 when Zoe is in kindergarten.
Summing up the experience over almost four years
“It was really lots of up and downs, lots of down,” said Ping.
“But we were still really grateful because infant leukaemia is really, really hard to treat and survival rate is really low. When she was diagnosed, she was given less than 20% chance of survival.

“She had infant ALL with a mutation called KMT2A rearrangement which makes the disease really aggressive and really hard to treat.
“Because I was in the [Facebook] support group, I see a lot of children with the same diagnosis didn’t make it.
“We’re really grateful for all the help and funding.”
Life after Zoe’s treatment
Life is now “pretty normal at this moment” for Zoe.
“She is really happy, but it’s been tough, and she has some delays in her development, especially in language, so she will be in a special school next year,” said Ping.
She urges other parents in a similar situation are to find other people who are having the same experience and “to know all the information, like as much as available to you”.
“Connect with people with the information and the same experience. It can really help you,” she said.
If you have found any content in this story difficult or challenging, we encourage you to take care of your mental health and wellbeing, and to seek the advice of your treatment team if you have any questions regarding your diagnosis, treatment or side effects. If you would like more information, emotional and practical support, feel free to call 1800 620 420 to be connected to your local Leukaemia Foundation blood cancer support coordinator. Any mention of medical treatments is not an endorsement.