Expert Series: Dr Susan Branford on molecular monitoring and drug resistance in CML
Professor Susan Branford is better known internationally than here in Australia where she heads a diagnostic lab in Adelaide, has research interests in CML, and is an NHMRC Research Fellow. Her work on the importance of molecular response in CML has been widely recognised and includes the International CML Foundation Prize in 2016 for outstanding contributions to the improvement of CML treatment in emerging economic regions, and the International Federation of Clinical Chemistry and Laboratory Medicine Distinguished Award in 2017 for significant contributions in molecular diagnostics.
Professor Susan Branford’s work on molecular monitoring and drug resistance, although largely behind the scenes, has underpinned many Australian and internationally significant developments in CML over the last 20 years.

The pathway to her current position as Head, Leukaemia Unit, Genetics and Molecular Pathology at SA Pathology, Centre for Cancer Biology wasn’t conventional. She started as a lab technician who worked in clinical chemistry for many years.
“That gave me a really good grounding in some of the key elements required to generate good diagnostic tests, which is what we are doing here in the lab now, as well as research,” said Dr Branford, also Professor, School of Pharmacy and Medical Science, at the University of South Australia.
In 2000, she took the opportunity to move to a new department–Genetics and Molecular Pathology–where her role was to develop methods using a new technique, real-time quantitative PCR* in various cancers. She worked with haematologist, Professor Tim Hughes, who had set up PCR when he was at Hammersmith Hospital in London.
“My role was to develop a technique and to start to monitor patients with chronic myeloid leukaemia, which we did. At that time imatinib [Glivec®] was first being tested,” said Dr Branford about the original, first generation tyrosine kinase inhibitor (TKI).
“After a few years of developing this method and being very interested in the research I was doing, Tim [Hughes] said, ‘look, I think the work you’re doing is at a PhD level, why don’t you apply to do a PhD?’, so I did.
“I’d already published papers at that stage and even though I didn’t have a primary degree, the university looked at my credentials and said ‘yes’ to my application, based on my publications and relevant background.”
Introducing molecular monitoring to the international stage

Dr Branford had an opportunity to participate in some exploratory research in patients who were treated with imatinib.
“Until imatinib was available, CML patients were either treated with interferon, which most patients couldn’t tolerate and only a few responded to, or patients had an allogeneic bone marrow transplant,” she said.
“Then imatinib, which is a targeted therapy, changed everything.”
“From the first trials, it was clear that patients were going to have very good responses,” said Dr Branford.
“Tim [Hughes] told Novartis that we had a method to monitor patients and we were able to perform exploratory molecular analyses for Australian and New Zealand patients enrolled in the IRIS international trial, that started in 2000.
“This trial enrolled over 1000 patients and was the first trial of newly diagnosed CML patients treated with imatinib.
“We worked with colleagues in London and Seattle who also had monitoring methods set up using real-time PCR for patients with CML. These labs performed the molecular analyses for the other patients enrolled in the IRIS trial. But our methods were all slightly different, which meant our results didn’t align. So we worked to standardise the results, and this was the first attempt to align data for CML patients generated by different labs.
“The trial protocol required that molecular analysis was only commenced once patients achieved a complete cytogenetic response.
“But we were lucky enough to get support to test all of the Australian and New Zealand patients at three-monthly intervals. This proved to be really informative because we monitored patients more intensively than a lot of the other patients on the trial,” she explained.
“We found that the achievement of a certain molecular response correlated with very good outcomes and the data was published in 2003,” said Dr Branford.
“Then we followed those patients who became resistant to imatinib, looking for their mechanisms of drug resistance. That’s really how it all started.”
Significance of Leukaemia Foundation funding support
The overall aim of Dr Branford’s research is to understand why some patients with CML don’t respond to therapy, given that most patients do extremely well.
“Patients can be treated with imatinib, the first generation drug and the least potent, and have very rapid responses. Some patients may eventually be able to stop therapy and maintain treatment-free remission,” she explained about a typical CML patient journey.
“But we know that some patients have a delayed response. By using molecular monitoring, we found that values very early into therapy are highly predictive of how patients are going to respond.
“A lot of our work is focused on trying to understand and to predict why some patients do well and why some patients have a poor response.”
Dr Branford, Professor Hughes, and Dr Deborah White received funding from the Leukaemia Foundation in 2008 that contributed to research with the primary goal of understanding the mechanisms of resistance and how to overcome this resistance to improve outcomes.
“At that time, we were very focused on mutations in BCR-ABL1. BCR-ABL1 is the primary genetic mutation that causes CML, and mutations in this fusion gene cause drug resistance. We were able to develop a very sensitive method to detect these mutations. We had some good publications from that work where we were able to show that low level mutations are clinically relevant.
“Any bit of funding we get means that we can do some analysis, even if it’s preliminary. We find these great preliminary results and we feed that back into our next grant application. It’s all been a fantastic support,” said Dr Branford.
Predicting treatment response
“We started off looking at BCR-ABL1 at diagnosis and found there was no predictive information; it didn’t matter what level you started with; it was what happened after treatment.
“By three months, if patients had a very rapid decline, they were going to do very well.
“We’ve always tried to find out what’s going on at diagnosis and it’s really starting to come together after many years of using new technology and looking outside of BCR-ABL1.
“We’re at quite an exciting spot.”
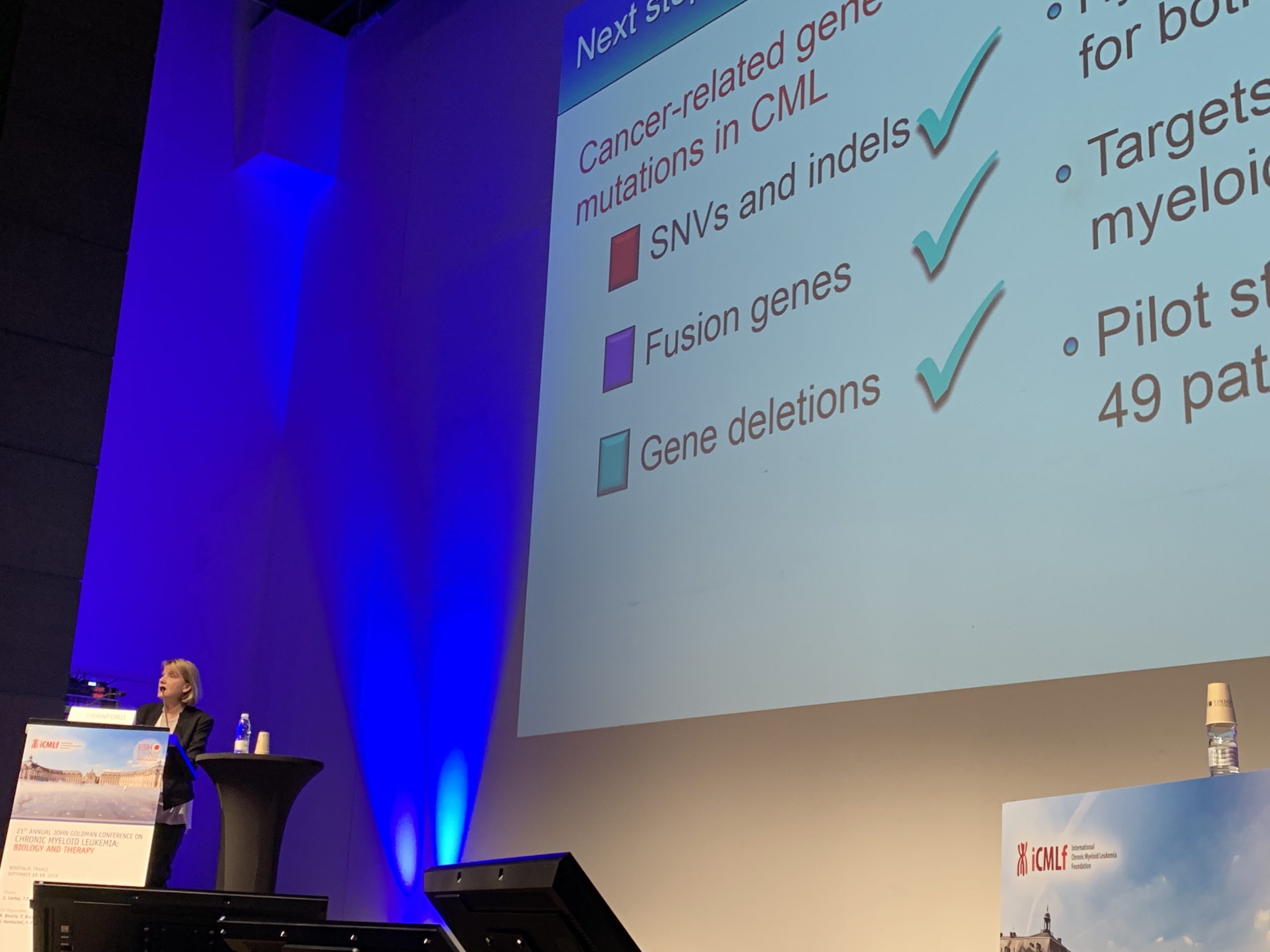
“We’re using new genomic and molecular techniques –whole exome sequencing**, or whole transcriptome sequencing–where we look at every gene at diagnosis.
“We did a pilot study that took us many years. We looked at patients who had the best responses and those who had the very worst responses. We found additional genomic abnormalities in some CML patients at diagnosis in addition to BCR-ABL1.
“These were mutations that are found in other types of leukaemia; in acute myeloid leukaemia and acute lymphoblastic leukaemia.
“Our study started in 2011 but even as far back as 20 years ago, scientists had detected the occasional mutation found in a highly mutated gene, like TP53.
“It wasn’t until the new sequencing technology came along that we could look at everything, and that we’ve really started to find these mutations.”
Dr Branford said the research has since been extended to an expanded cohort of CML patients, not just those with very poor or very good responses to imatinib. We are studying patients enrolled in the TIDEL II study, which was set up by Dr David Yeung and run out of Adelaide in conjunction with the Australasian Leukaemia & Lymphoma Group (ALLG). The results of that study were published in Blood in 2015. Blood is the top-ranking journal that publishes data on blood cancers.
“So far, in our preliminary work, it holds up that if patients have a mutation at diagnosis, then it puts them at a higher risk of treatment failure.
“PhD student and haematologist, Dr Naranie Shanmuganathan presented our preliminary data in early December [2020] in an oral session at the American Society of Hematology (ASH) meeting, which was a virtual meeting last year.
“We tested the diagnosis samples of patients where we know their outcomes; we know which patients did well and which patients did poorly.
“We’ve looked at the genomics at diagnosis of about two-thirds of the patients so far and have found that having these mutational events at diagnosis is an independent predictor of poor outcome.
“At a live question time after Dr Shanmuganathan’s presentation, one of the questions was, ‘when is this going to be available in the clinic?’.
“That was quite exciting for us, to hear that there is interest from around the world.”
“There is still a lot of work to do. We need to find out if the poor risk conferred by mutations at diagnosis can be overcome with more potent inhibitors.”
Dr Branford said the next step now is to go back and test the tissue samples (usually peripheral blood) of other CML patient cohorts–those treated with the more potent inhibitors such as nilotinib (Tasigna®) and dasatinib (Sprycel®) as their first line of therapy–to see what their outcomes have been.
“That could be quite useful,” she said.
“If we find that a patient has a particular mutation at diagnosis and is treated with a certain drug that reduces the risk of treatment failure, then that could be really important. It could be practice changing in terms of helping clinicians decide the best drug to give at diagnosis.
“Our aim is to identify those patients who will do really well on the standard dose of imatinib, which is a safe drug, whereas the more potent inhibitors (nilotinib and dasatinib) have some toxicity and cardiovascular risk associated with them, so the patients who have those drugs need to be carefully selected.
“But that’s another year or so off until we get those results.
“We’ve got patient consent for this work, it’s just a matter of funding.
“Getting funding is becoming harder and harder and, unfortunately, there may be a time when we just aren’t able to pursue the things we would like to do, based on our preliminary data, because we just don’t have funds.”

Retrospective analysis using archived tissue samples
For a lot of this research, Dr Branford uses existing samples that have been collected and stored for many years in Adelaide.
“Patients with CML are routinely monitored for BCR-ABL1, and we do a lot of the molecular analysis for Australian clinical trials.
“We’ve got about 700 patients who we’ve followed in clinical trials.
“It’s a great resource,” she said.
“We correlate the data with the BCR-ABL1 values we’ve collected over time.”
Groups around the world are finding that tissue banks of stored patient samples, where the response to treatment is known, can provide a wealth of information.
“It’s a very nice retrospective analysis,” said Dr Branford.
“One of the initial mechanisms of drug resistance we found were mutations that occurred within the BCR-ABL1 gene itself, in the drug-binding site.
“Again, with this rich data source, we were able to go back, track, and correlate the emergence of these mutations with drug resistance.
‘We’ve moved on from there and are now looking more broadly at other mutations and other genes,” she said.
Several other groups around the world developed molecular monitoring techniques and established these rich data resources at around the same time; the Hammersmith in London; in Germany; and Jerry Radich’s group in at Seattle in the U.S.
World first trial for asciminib has opened
Hopefully, new samples will be added to the CML tissue bank in Adelaide from the 100 participants who are expected to enrol in a new national study that opened in late 2020.
“I think this is the first clinical trial in the world treating newly diagnosed patients with a new drug, called asciminib,” said Dr Branford about the ALLG CML13 study, also known as the ASCEND trial, run from Adelaide.
Asciminib, previously known as (ABL001) is another drug that targets BCR-ABL1, but it is different because its activity is very specific.
“It has limited off-target activity, so has limited toxicity. We’re very excited to be able to test and treat patients with asciminib as their first line of therapy.”
But Dr Branford said her research group doesn’t have the necessary funding to test these patients at diagnosis.
“We keep applying to various funding bodies to get the money to do the testing. The patients will all be consented to do the test, it’s just dependent on if we can get some funding,” she explained.
“This trial might recruit very quickly because, at the moment, this drug is not available outside of a clinical trial.”
Data on asciminib was presented at ASH in a late-breaking abstract session on the results of a large randomised Phase III trial, called ASCEMBL, for patients who had failed prior therapy; up to three different therapies.
“This drug met its primary endpoint, meaning it was superior to the other drug that was used in the trial – that’s very exciting,” said Dr Branford.
“It’s now gone in for fast track approval to the FDA [in the U.S.] as the second line therapy as a monotherapy.”
Dr Branford said we will have some idea how well patients respond to asciminib very early in the ASCEND trial and there is a treatment intervention timeline.
“By three months, if the patient hasn’t reached a certain level of BCR-ABL1, then the study has built in some treatment intervention at that stage.

Investigating the effect of mutations on therapy response
While Dr Branford heads a diagnostic lab, her focus is research, which involves grant writing and paper writing [for submission to journals], and involvement in clinical trials.
“We’ve worked with Novartis over a number of years. They have an interest in these mutations that cause resistance.
“Over the last few months, we have been testing samples of patients enrolled in the ASCEMBL trial at the time just before they start their asciminib; we’re looking at what mutations they have, and we’re starting to get data from this clinical trial.
“We will do an exploratory analysis, to see the effect of these cancer gene mutations on response to asciminib. This will be a companion analysis to that in the TIDEL II trial,” said Dr Branford who, since 2018, has been writing up the trial methodology and has performed validation studies.
“We’ve got a huge amount of data and we’re analysing the last of our data for the TIDEL II study. We’ll do the statistics on that, and that will be the next paper we work on.”
Rolling out molecular testing across the globe
Dr Branford considers her greatest contribution to science is developing the molecular techniques and being involved in rolling out the test globally.
“It is now accepted that this is how patients should be monitored,” she said.
“Over the last decade, once we demonstrated that there was a clinically relevant reason for doing molecular analysis, labs have taken this up. We had to work hard as an international community with collaborators to standardise methods.
“It took many, many years… a lot longer than we thought, because the technique is quite complex and lots of things can lead to variability.
“Now it’s routine that all labs offer molecular testing for CML, whereas if we look back five or six years ago, that wasn’t the case.
“It is much harder in undeveloped countries and we’ve been working with commercial groups, including Cepheid, which developed an instrument called the GeneXpert.
“Again, this has been a work in progress over the last decade.
“GeneXpert is a very rapid cartridge-based method that’s used in a lot of labs in places like Africa and India, where patients can’t access drugs unless they have a definitive CML diagnosis.
“GeneXpert has come to prominence in the COVID era because this instrument is being used for rapid COVID testing, but it also does rapid BCR-ABL1 testing.”
The importance of molecular monitoring
In the first molecular monitoring study Dr Branford did, in the IRIS trial, she found that if patients reached a certain level of BCR-ABL1 after 12 months of therapy, they were essentially protected from disease progression.
“It’s now known as a safe haven, and it’s got its own term, it’s called a major molecular response,” she said.
“It’s the equivalent of a three-log reduction from the diagnosis level. That was the first time that this was found to be an important response.
“Now, in most clinical trials, the primary endpoint is the achievement of a major molecular response and if that can be achieved within 12 months of therapy these patients will have a very good outcome.
“A lot of groups then looked at earlier time points and we’ve now found that if patients reach a BCR-ABL1 ratio of 10% at three or six months, then this has prognostic information. If patients don’t reach these levels, we know that those patients are at risk of treatment failure, disease progression, or even death.
“We now have molecular milestone values at three, six, and 12 months, and these are now our decision points.”
Dr Branford said that in 2013, international recommendations for monitoring patients with CML, published by the European LeukemiaNet, for the first time recommended that molecular milestone values are used for treatment decisions.
“Very early molecular monitoring is important because it can determine whether clinicians should change therapy so that patients have a chance of achieving an optimal response,” she said.
“If BCR-ABL1 values are greater than 10% at three months, the recommendation is to confirm the result by doing another test very rapidly. And if it’s still greater than 10, that’s a bad sign. That’s when the recommendations mandate a change of therapy. Otherwise those patients are at high risk of disease progression. It’s become very important.”
Greatest unmet need in CML
Dr Branford thinks the greatest unmet need in CML is finding appropriate therapy for patients whose disease advances to a rapidly fatal blast crisis. This only occurs in a small number of patients now.
“There are some patients who progress very rapidly,” she said.
“We recently had a young person here who was diagnosed in the chronic phase, started standard therapy, and unexpectedly went straight into blast crisis. Very sad. The patient will have an allogeneic transplant.”
“Tyrosine kinase inhibitors are not effective for patients with disease progression and there is no other effective drug therapy,” said Dr Branford.
“Their best chance is to have chemotherapy, to ablate the leukaemia, then go on to have a transplant. Fingers crossed for this most recent patient.”
Between five and 10% of patients fit into this category, depending on the drug they start their treatment with.
“There’s less progression if patients start with the more potent inhibitors, but these are associated with greater toxicity. There’re pros and cons, and these are the issues their clinicians are dealing with at the time of diagnosis; what’s the best drug for their patient?”
When Dr Branford finishes all the current preliminary work looking at diagnosis, she hopes to focus her research on this group of patients.
“Maybe, if we can introduce rapid genomics at diagnosis, we can work out what are these mutations that are leading to this very rapid progression.
“Maybe it will identify those patients who perhaps need a more potent inhibitor, and they should start to look for a [bone marrow] donor very early,” she said.
“If we can identify a mutation, like IDH1, which we’ve seen occasionally in CML, and which we know occurs in acute myeloid leukaemia, we know there are inhibitors for that.
“As more and more drugs are developed that target specific mutations, there may be effective treatment for these patients.”
Ongoing developments in CML
Dr Branford said that, in addition to the asciminib trial and the research using genomics, a “very exciting area of research is trying to understand how we can pick patients who are going to be successful when they stop therapy; that is, patients with treatment-free remission”.
“I’ve been fortunate enough to be involved in international patient advocate groups because of our international connections,” she said.
“Following on from our work, and other groups’, where we are looking at genomics in CML, Tim and I formed the International Genomics Alliance, which was launched in 2018, to eventually pool all of our data, and we are working closely with patient advocates.
One over-arching group, called the CML Advocates Network, has connected 125 CML patient groups worldwide, and is working with academics and pharmaceutical companies to work out goals and spread word of the latest research findings.
Dr Branford worked with two international patient advocates who are both in treatment-free remission and who helped review her most recent grant application.
“It’s becoming more and more important that we work closely with patients, and that they review our grant applications,” she said referring to what is acceptable to the patient community, such as the level of drug toxicity.
“There are some drugs that are highly toxic,” she said.
“Modification of our grant applications based on feedback from patients is going to be important to improve overall outcomes for patients.”
* Polymerase chain reaction (PCR) is a technique used to amplify small segments of DNA because significant amounts of a sample of DNA are necessary for molecular and genetic analyses.
** Whole exome sequencing sequences the 1.5% of the whole human genome that codes for proteins. Whole transcriptome sequencing sequences the RNA and can measure gene abundance.
Last updated on January 3rd, 2023
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.